Clinical Impact of Coronavirus Disease 2019 Outbreaks in Korea on Seizures in Children
Article information
Abstract
Purpose
Coronavirus disease 2019 (COVID-19) can be associated with neurological complications. This study investigated the impact of COVID-19 outbreaks on seizure incidence and duration in children in Korea.
Methods
We retrospectively analyzed medical records from Kyungpook National University Children’s Hospital, including 768 children with seizures during the peak COVID-19 outbreaks in March and August 2022, and compared patterns with the same periods in 2021. We examined demographic and clinical characteristics, causes of seizures, underlying conditions, seizure durations, and COVID-19 test results.
Results
Out of 16,373,836 COVID-19 cases during the first peak, 25.6% were children (4,184,383), and during the second peak, 20.5% of 6,400,244 cases were children (1,314,331). No significant age differences were observed between either peak and the previous year. However, when compared to the previous year, febrile seizures (FS) were more common during both peaks (25.9% vs. 65.1% in the first peak; 34.3% vs. 59.2% in the second peak). The prevalence of FS was significantly higher in the COVID-19-positive group (84.1%) than in the COVID-19-negative group (51.9%). The incidence of new-onset seizures or breakthrough seizures showed no significant difference. Seizure duration and the incidence of status epilepticus (SE) showed no significant changes, but SE was more common in the COVID-19-negative group (17.1% vs. 6.2%). The clinical features of FS were similar in both groups.
Conclusion
COVID-19 appeared to increase the risk of FS in children, but there was no significant impact on the risk of breakthrough seizures or SE in children with epilepsy. Nevertheless, larger-scale studies are necessary.
Introduction
Coronaviruses, including severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2, the causative agent of coronavirus disease 2019 [COVID-19]), are a group of RNA viruses that cause respiratory infections. First identified in China in late 2019, SARS-CoV-2 is a novel coronavirus linked to neurological symptoms as well as respiratory issues. The major neurologic manifestations during acute COVID-19 include headache, seizures, dizziness, stroke, Guillain-Barré syndrome, acute disseminated encephalomyelitis, nerve palsies, anosmia, and multisystem inflammatory syndrome [1-4]. Since January 2022, the Omicron variant has been dominant in Korea, with two peak outbreaks in March and August of 2022 that led to a rapid increase in the number of patients with seizures [4].
The putative mechanism of COVID-19 that causes seizures is linked to direct viral injury to neural cells and to inflammation. The neurotropic nature of COVID-19 induces neural infection through angiotensin-converting enzyme 2 in brain endothelial cells, triggering a cascade of inflammation mediated by cytokines [5-7]. These hyper-inflammatory responses induced by COVID-19 increase neurological excitability, making children more susceptible to experiencing febrile seizures (FS) [8,9].
This study assessed the impact of COVID-19 on the incidence and duration of seizures in children by comparing two peak outbreaks with corresponding periods from the previous year when COVID-19 was rare in children.
Materials and Methods
1. Study population and data
We conducted a retrospective review of the medical records at Kyungpook National University Children’s Hospital (KNUCH) of patients with seizures during the peak outbreaks of the COVID-19 pandemic in March and August 2022. KNUCH provides care for the region that includes Daegu and its surrounding areas, with a total population exceeding 5 million people. A comparison was made between the two peak periods of 2022, when COVID-19 was prevalent in children, and the same periods in 2021, when COVID-19 was rare in this demographic. Out of 852 children initially considered, 768 were included in the study after excluding those with insufficient records and those with multiple daily visits (i.e., duplicate cases). Patients’ demographic and clinical characteristics were analyzed, as well as the etiology of the seizures, underlying conditions, seizure duration, and COVID-19 test results. We defined FS as seizures in children aged 3 months to 5 years associated with febrile illness, not related to a central nervous system infection, and without a history of previous neonatal seizures or unprovoked seizures. A new-onset seizure was defined as an afebrile seizure without a history of previous unprovoked seizures that did not meet the criteria for FS. In addition, epileptic seizures were defined as seizures in patients who were previously diagnosed with epilepsy at our hospital or another hospital. Status epilepticus was defined as ongoing seizures that required anti-seizure medication before and/or during a visit to the emergency room (ER) at our hospital or another hospital. A positive COVID-19 test was determined by either a positive rapid antigen test or polymerase chain reaction test.
This study received approval from the Institutional Review Board of KNUCH (KNUCH 2024-01-011). Given the retrospective nature of the study and its non-adverse impact on the rights and welfare of the subjects, the requirement for written informed consent from patients was waived.
2. Statistical analyses
Statistical analyses were performed using SPSS version 18.0 (SPSS Inc., Chicago, IL, USA). For continuous variables such as the patient’s age (in months) and the duration of seizures, the independent t-test was used for normal distributions, and the Mann-Whitney test was used for non-normal distributions. The chi-square test or Fisher exact test was used for categorical data such as gender, use of anti-seizure medication in the ER, cause of seizures, and type of seizures. In all analyses, P values <0.05 indicated statistical significance.
Results
1. Overall trend of COVID-19 outbreaks in Korea
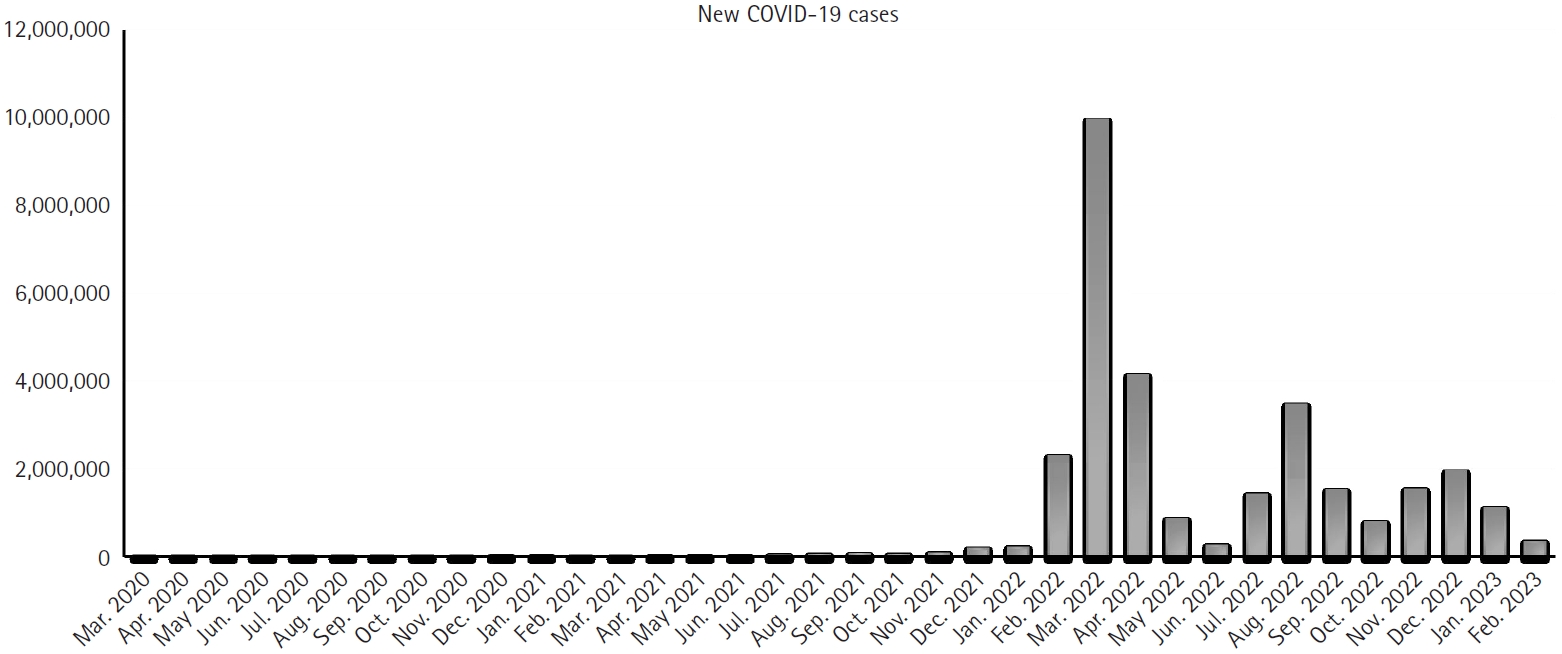
The first case of COVID-19 in South Korea was reported on January 20, 2020. By February 21, 2020, there were 346 confirmed cases, according to the Korea Disease Control and Prevention Agency (KDCA). South Korea, known for its well-organized epidemic control programs along with Singapore and Taiwan, experienced a major spike in cases related to the Omicron variant in early 2022, with 170,000 cases reported on February 22. Social distancing rules began to relax on March 4, 2022, and a shift toward endemic living was declared on March 18. Consequently, there were 9,962,498 new confirmed COVID-19 cases in March 2022 and 3,472,043 cases in August 2022, indicating two peak outbreaks (Fig. 1) [10-12].
2. COVID-19 outbreaks and their variables
We compared the periods of February to April 2022 and July to September 2022, when COVID-19 was prevalent in children, to the same periods the previous year, when COVID-19 in children was rare. In the period February to April 2021, with no predominant variants, there were 43,506 cases, of which 12.8% were children <19 years old. The Delta variant was predominant in the July to September 2021 period when 153,562 cases were reported, 16.6% of which were children. From February to April 2022, the Omicron variant (sublineages BA.1 and BA.2) predominated, with 16,373,836 cases reported, of which 4,184,383 (25.6%) were children. From July to September 2022 when the Omicron variant (BA.5) predominated, there were 6,400,244 cases, of which 1,314,331 (20.5%) were children (Table 1) [10-12].
3. Comparing the demographic and clinical characteristics of the first peak to the previous year
In a comparison of the time periods February to April 2021 and February to April 2022, there were no significant differences in the male-to-female ratio (P=0.644), the patients’ mean age (64.77 months vs. 56.21 months, P=0.935), and the duration of seizures (7.74 minutes vs. 6.60 minutes, P=0.517) between the two groups, respectively. In addition, there was no significant difference in the number of patients requiring anti-seizure medications after arriving at the ER (26 [12.4%] vs. 13 [12.0%], respectively; P=0.918). Cases of FS were significantly higher in the February to April 2022 group (136 [65.1%]) than in 2021 (28 [25.9%]) (P<0.001), while new-onset seizures were significantly higher in the February to April 2021 group (41 [38.0%] vs. 33 [15.8%]; P<0.001). Epileptic seizures were also significantly more common in the group from February to April 2021 (34 [31.5%]) than in 2022 (31 [14.8%]) (P<0.001). However, there were no significant differences in seizure type between the 2021 and 2022 groups: generalized seizures (73 [68.9%] vs. 122 [75.8%], respectively; P=0.213), and focal seizures (4 [3.8%] vs. 4 [2.5%], respectively; P=0.717) (Table 2).
4. Comparing demographic and clinical characteristics during the second peak to the previous year
Comparing the mean ages for July to September 2022 (53.40 months) with same period of the previous year (70.97 months), the 2022 group was significantly younger (P=0.036). However, there was no significant difference in the male-to-female ratio (P=0.835). The mean duration of seizures was 7.62 and 6.25 minutes, respectively, showing no significant difference between the two groups (P=0.393). Similarly, there was no significant difference in the number of cases of status epilepticus (25 [8.0%] and 7 [5.0%], respectively; P=0.322). Whereas, the number of FS cases was 48 (34.3%) in the July to September 2021 group versus 184 (59.2%) in the July to September 2022 group, a significant difference (P<0.001). However, the rates of new-onset seizures and epileptic seizures were significantly higher in the July to September 2021 group than in the same period in 2022 (P<0.001, P=0.017, respectively). No significant differences in the rate of generalized and focal seizures were identified: generalized seizures in 2021 (99 [72.3%]) versus 2022 (207 [80.2%]) (P=0.213), and focal seizures in 2021 (5 [3.6%]) versus 2022 (10 [3.9%]) (P=0.911) (Table 3).
5. Comparing the demographic and clinical features of the COVID-19-negative group and the COVID-19-positive group
During the four periods, 329 children underwent COVID-19 testing. Among them, 113 children tested positive, while 216 tested negative. In a comparison of the negative to-positive groups, there were no significant differences in the male-to-female ratio (P=0.069), mean age (45.47 months vs. 49.47 months, respectively; P=0.431), and duration of seizures (9.93 minutes vs. 6.57 minutes, respectively; P=0.378). However, the rate of status epilepticus was higher in the COVID-19-negative group (37 [17.1%] vs. 7 [6.2%], P=0.006). The rates of new-onset seizures and epileptic seizures were also higher in the COVID-19-negative group: (46 [21.3%] vs. 5 [4.4%], P=0.002) and (46 [21.3%] vs. 8 [7.1%], P<0.001), respectively. Conversely, the rate of FSs was higher in the COVID-19-positive group (95 [84.1%]) than in the negative group (112 [51.9%]) (P<0.001). There were no significant differences in seizure type between the two groups (Table 4).
6. Comparing the demographic and clinical features of FS between the COVID-19-negative group and the COVID-19-positive group
Comparing patients with FS based on their COVID-19 test results, the monthly age was significantly higher in the COVID-19-positive group than in the negative group (41.8 months vs. 26.8 months, P=0.001), with no significant difference in the male-to-female ratio. In addition, differences in the duration of seizures (4.4 minutes vs. 5.3 minutes, P=0.531) were not significant, nor were the rates of status epilepticus (5 [5.3%] vs. 7 [6.3%], P=0.762). Generalized FS occurred more frequently in the COVID-19-negative group than in the positive group (87 [84.5%] vs. 50 [71.4%], P=0.038) (Table 5).
Discussion
An increasing number of pediatric cases with neurological manifestations of COVID-19 have been reported, although these are less common than in adults. However, the neurological complications in children can vary based on patient age and underlying conditions. The data on clinical features, particularly neurological manifestations, and prognostic factors are still limited. This study focused on the impact of COVID-19 on seizures in children by comparing the two peak outbreaks in 2022 with the corresponding periods from the previous year in Korea.
The World Health Organization classified coronaviruses as Alpha, Beta, Gamma, Delta, and Omicron based on mutations in the gene encoding the spike protein. In Korea, the detection rate for Alpha, Beta, and Gamma mutations did not exceed 50% [10,12]. However, after the Delta and Omicron mutations were introduced, there were large-scale outbreaks of COVID-19, with two peaks occurring when Omicron mutations were predominant. During the previous year, no dominant virus was observed in the period that coincided with the first peak in 2022, while the Delta variant was dominant in the period that coincided with the second peak [10-12].
This study showed that the proportion of pediatric patients increased during the period when Omicron variants were dominant in 2022 compared to when Delta variants were dominant in 2021. We attribute this phenomenon to limited vaccination in children and the strong transmissibility of the Omicron variants. Initially, the KDCA recommended COVID-19 vaccination for pediatric patients with high-risk conditions, including chronic medical diseases, neuromuscular diseases, and immunocompromised conditions. However, the recommendation expanded to include all 12- to 17-year-old adolescents in mid-October 2021. For high-risk 5- to 11-year-olds, vaccination was recommended in late March 2022 during the peak of the Omicron surge. Vaccination for healthy children aged 5 to 11 years was left to parental choice [13].
Previous studies on the frequency of FS in relation to COVID-19 variants reported that Delta variants had no or minimal effect on FS. However, the frequency increased with the emergence of Omicron variants [14-17]. Our study showed a similar significant increase in the rate of FS during the two peak periods when Omicron variants were predominant.
Regarding the impact of COVID-19 on breakthrough seizures in people with epilepsy, it has been shown that COVID-19 exacerbates seizures in adults but does not appear to do so in children [18-21]. Although there was no notable difference in the rate of breakthrough seizures during the two peak periods in our study, statistically lower rates of new-onset seizures and epileptic seizures were observed during these periods. While previous studies indicated that COVID-19 was associated with a higher likelihood of provoked seizures and status epilepticus in both children and adults [22,23], our findings indicated no significant difference in occurrence rates during the two peak periods. Surprisingly, our study revealed statistically lower rates in the COVID-19-positive group. We attributed this to the limited social activities of patients with epilepsy, which may have influenced the number of COVID-19 infections.
Male gender has emerged as a risk factor in FS [24,25]. Consistent with prior studies, our study revealed a higher frequency of FS in males, observed in both the COVID-19-positive and COVID-19-negative groups. In a previous study, it was demonstrated that the group with COVID-19-related FS had a higher mean age than the COVID-19-negative group [17]. Our study found similar results; we observed a higher mean age in the COVID-19-positive group. The reason for this may be that many viral diseases, including roseola infantum, commonly infect children under 2 years of age. In a particular study, although lacking statistical significance, the COVID-19-positive group exhibited longer seizure duration, multiple seizure episodes, and a higher prevalence of complex FS [17]. However, in our comparison of FS in COVID-19-negative and COVID-19-positive groups, no significant differences were found in seizure duration, prevalence of complex FS, and frequency of emergent anti-seizure medication use between the two groups. Consistent with a previous study, generalized seizures constituted the majority of FS associated with COVID-19 [14].
Acute symptomatic seizures are seizures that occur in close temporal association with acute central nervous system disorders, including metabolic, toxic, structural, infectious, or inflammatory disorders. In this study, there were cases of benign convulsions with mild gastroenteritis, hyponatremia, subdural hemorrhage, cerebral concussion, autoimmune encephalitis, and meningoencephalitis. COVID-19 infection did not affect the occurrence of symptomatic seizures.
This study had certain limitations. It was a single center, retrospectively-designed study, which potentially introduced selection bias into the incidence and clinical spectrum. In addition, the possibility of coinfection with other viruses alongside COVID-19 could not be ruled out. Despite these limitations, the study provided insight into the impact of COVID-19 on seizures in children. We believe that further systematic and large-scale studies are necessary to confirm these findings.
In conclusion, COVID-19 seems to increase the risk of FS in children, but no significant impact was observed on the risk of breakthrough seizures in children with epilepsy or on the occurrence of status epilepticus.
Notes
Soonhak Kwon is an editor-in-chief of the journal, but he was not involved in the peer reviewer selection, evaluation, or decision process of this article. No other potential conflicts of interest relevant to this article were reported.
Author contribution
Conceptualization: SK. Data curation: SL and SK. Formal analysis: SL and SK. Methodology: SL and SK. Project administration: SL, SKH, YJL, HWB, and SK. Visualization: SL, SKH, YJL, HWB, and SK. Writing - original draft: SL and SK. Writing - review & editing: SL, SKH, YJL, HWB, and SK.