 |
 |
- Search
| Ann Child Neurol > Volume 29(1); 2021 > Article |
|
Acute necrotizing encephalopathy (ANE) of childhood is characterized by encephalopathy presenting with symmetrical multiple necrotic brain lesions along with multiple organ involvement. Affected children often present dramatic and profound neurologic deficits after prodromal viral infection symptoms. We report a case of a 4-year-old boy with acute necrotizing encephalitis related to Mycoplasma pneumoniae who managed to recover from severe neurocognitive impairment. A previously healthy 4-year-old boy had traveled around America and Spain for 1 month. Ten days after return, he had fever due to acute pharyngotonsillitis. On the third day of fever, he experienced abdominal pain, vomiting, and a generalized tonic seizure. He was transferred to the emergency room with an on-going seizure of 30 minutes which ceased after injection of lorazepam.
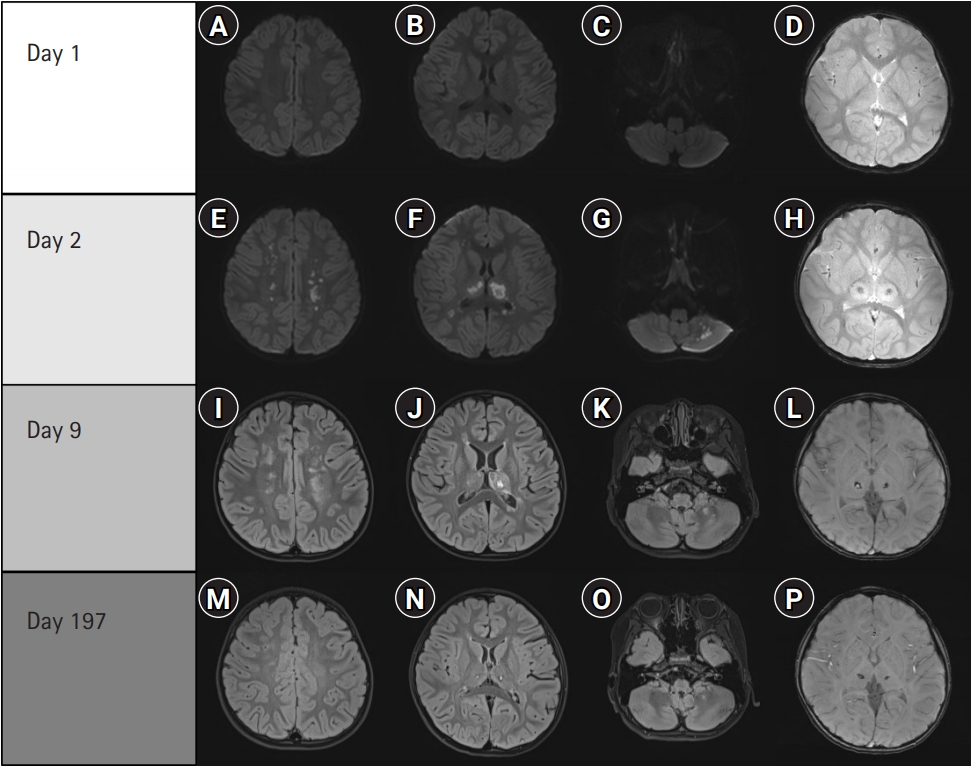
The patient was drowsy but cranial nerve exam, pupillary light reflex, and extraocular movements were normal. Overall motor and sensory function was intact. Within 2 hours of admission the patient had three vomiting episodes. The initial diffusion-weighted brain magnetic resonance imaging (MRI) showed no diffusion-restriction lesions and the intrathecal pressure was normal. Blood and cerebrospinal fluid (CSF) tests, renal parameters, electrolyte levels, and urine analysis were also normal. Chest radiograph showed mild bilateral peribronchial infiltrations. The patient was then admitted to the intensive care unit. Next morning, his Glasgow coma scale (GCS) was 6 (eye opening 1, verbal response 2, and motor response 3). He showed generalized rigidity of extremities and no response to pain. Intubation was done to obtain respiratory stability. Clinically suspecting encephalitis, intravenous immunoglobulins (IVIG; 500 mg/kg/day, for 5 days) and high-dose methylprednisolone pulse therapy (30 mg/kg/day, for 3 days) were immediately started. Repeated brain MRI showed symmetric diffusion restriction and T2 high-signal intensity at both thalami. Inside the thalamus, the gradient recall echo showed low-signal intensity, indicating possible hemorrhagic lesions. Abrupt changes were seen in less than a day, which gradually resolved (Fig. 1). We diagnosed him with ANE. Empirical cefotaxime, vancomycin, and acyclovir were administered. Following the general tonic seizure on the second day, the patient had five consecutive seizure episodes. Fosphenytoin and levetiracetam were administered. Continuous electro-encephalography showed delta waves on background exhibiting nonspecific diffuse cortical dysfunction, but no epileptiform discharges.
The CSF culture, viral and bacterial multiplex polymerase chain reaction (PCR) tests were negative. Real-time PCR from nasopharyngeal swab was negative for human adenovirus, bocavirus, coronavirus, enterovirus, influenza A/B, metapneumovirus, parainfluenza virus, rhinovirus, and respiratory syncytial virus. Serologic tests for herpes simplex virus, mumps virus, Epstein-Barr virus, cytomegalovirus, varicella-zoster virus, and Japanese encephalitis virus were all negative except M. pneumoniae. The immunoglobulin M (IgM) titer of M. pneumoniae on hospital day 1 was 416.89 U/mL (cutoff level, 71 U/mL), which fell to 363.98 U/mL on day 11 and 54.11 U/mL on the 8-month follow-up. Stool culture, viral and bacterial panel results were also negative. Empirical cefotaxime and vancomycin were switched to azithromycin.
For 4 days, the patient maintained a GCS score between 5 and 6 and required mechanical ventilation. On hospital day 5, his GCS score recovered to 10 (spontaneous eye opening 4, incomprehensible sounds 2, withdrawal response to pain 4). On hospital day 43 at discharge, his motor power of upper extremities had recovered to grade 3 and lower extremities to grade 2. Sensory functions were not testable. He had grade 3 deep tendon reflexes, and all four limbs showed some rigidity. He could comprehend spoken words but had difficulty in expressing himself. All the results from whole exome study including pore protein ran binding protein 2 (RANBP2) gene, recently known for its correlation with familial autosomal dominant ANE [1] were normal. On last follow-up at 8 months, he had recovered fully in all developmental domains, except for gait disturbance and generalized intentional tremor predominant on the left side. Dyskinesia, slow speech, and tremor were improved by levodopa. Subsequent brain MRI on day 197 showed resolution of the ANE.
The ANE is generally thought to occur via three main mechanisms: direct neuroinvasion, neurotoxin, and most of all, infection leading to immune dysfunction [2]. Typically, a viral or bacterial infection precedes ANE. M. pneumoniae can also lead to extrapulmonary manifestations including central nervous system (CNS) complications. In a study of 1,988 patients in the California Encephalitis Project, M. pneumoniae was the most common agent implicated in encephalitis, especially in children [3]. They were diagnosed primarily by the elevation of M. pneumoniae IgM in the blood. PCR and antibodies in CSF were rarely positive [3]. Qualitative measurement of IgM has only moderate sensitivity, but serial testing in our patient revealed peak levels at hospital day 1 and then a gradual decrease which turned to negative after 8 months, strongly implying that M. pneumoniae may be responsible.
ANE is often associated with significant morbidity. Although clinical usefulness of the immunomodulating therapy has not been confirmed, early IVIG and steroid pulse therapy is thought to be associated with better outcomes [3,4].
Antimicrobial therapy for M. pneumoniae is more controversial. The resistance against macrolides has increased from 51.1% in the 2011 epidemic to 87.2% in 2015 [5]. Unless the patient responds to macrolides, second line antibiotics should be considered.
Our patient at last follow-up showed only a slight limitation in fine motor movement on the left. He underwent rehabilitation therapy, lasting up to 4 hours per day, for 7 months. Whether his improvement was due to the early immunomodulating therapy or the rehabilitation program is not clear, but rehabilitation should be strongly encouraged.
In summary, we describe a patient infected with M. pneumoniae who underwent a fulminant clinical course requiring intubation and intensive care unit care. In general, M. pneumoniae infection is benign, but CNS involvement is not so rare, and in some cases can lead to severe ANE. Despite the early detection with brain MRI and administration of immunomodulating therapy and antibiotics, the patient manifested severe neurocognitive impairment. Early immunomodulating therapy is thought to be beneficial, with some but not strong evidence. Fortunately, intensive rehabilitation is highly effective in children. Therefore, in combination with immunomodulating therapy, we strongly recommend an intensive rehabilitation program for patients with neurocognitive sequelae.
This study was approved by the Institutional Review Board of Korea University Anam Hospital (approval number: 2020AN0471). Written informed consent by the patients was waived due to a retrospective nature of our study.
Conflicts of interest
Baik-Lin Eun is an editorial board member of the journal, but he was not involved in the peer reviewer selection, evaluation, or decision process of this article. No other potential conflicts of interest relevant to this article were reported.
Notes
Author contribution
Conceptualization: BLE and JHB. Data curation: SHP, SO, and JHB. Formal analysis: SO and JHB. Funding acquisition: BLE and JHB. Methodology: BLE and JHB. Project administration: SHP and JHB. Visualization: BLE and JHB. Writing-original draft: SHP. Writing-review & editing: SHP, BLE, and JHB.
Acknowledgments
This work was supported by National Research Foundation of Korea grant (NRF-2019R1G1A1100508) and by Korea University Hospital Hin Moe (Prof. Hyun-Gum Lee) Research Fund.
Fig.┬Ā1.
(A, B, C). No evidence of diffusion restriction on diffusion weighted imaging. (D) No evidence of acute hemorrhage on T2 fast field echo (FFE). Diffusion restriction on (E) white matter, (F) thalami, and (G) cerebellar hemisphere. (H) Low signal intensity on gradient echo sequence (T2 FFE) indicates hemorrhage. Patchy, nodular high signal intensity on T2 fluid-attenuated inversion recovery in the (I) periventricular white matter, (J) thalami and (K) cerebellar hemisphere. (L) Susceptibility weighted imaging of the thalami. (M, N, O, P) Evolving acute necrotizing encephalitis.
References
1. Denier C, Balu L, Husson B, Nasser G, Burglen L, Rodriguez D, et al. Familial acute necrotizing encephalopathy due to mutation in the RANBP2 gene. J Neurol Sci 2014;345:236-8.


2. Guleria R, Nisar N, Chawla TC, Biswas NR. Mycoplasma pneumoniae and central nervous system complications: a review. J Lab Clin Med 2005;146:55-63.


3. Christie LJ, Honarmand S, Talkington DF, Gavali SS, Preas C, Pan CY, et al. Pediatric encephalitis: what is the role of Mycoplasma pneumoniae? Pediatrics 2007;120:305-13.









