Prevalence of Pediatric Autism Spectrum Disorder in Korea Using National Statistics Including the COVID-19 Pandemic, 2011 to 2021
Article information
Abstract
Purpose
Regularly analyzing the prevalence of autism spectrum disorder (ASD) is important to inform policies and strategies for proper management. The present study aimed to esti-mate trends in ASD prevalence according to age and time in Korean children.
Methods
We monitored the annual prevalence of ASD in children aged 2 to 18 years based on information from Statistics Korea and the Korean National Health Insurance Service. We estimated changes in prevalence between 2011 and 2021 after stratifying partici-pants into three age groups. Furthermore, we analyzed the prevalence of ASD by birth year.
Results
The highest level of prevalence appeared in children aged 6 years, and thereafter, it de-clined with age. The prevalence of ASD in children aged 2 to 18 years increased from 0.05% in 2011 to 0.12% in 2021. During the same time, the prevalence in preschool children (2 to 5 years) remarkably increased from 0.04% in 2011 to 0.12% in 2021, while the prevalence in adolescents (13 to 18 years) increased from 0.05% in 2011 to 0.09% in 2021. The prevalence of ASD notably increased during the coronavirus disease 2019 (COVID-19) pandemic (2020 to 2021). Among children born between 2011 and 2015, the prevalence of ASD was higher for children with recent birth years, especially during the COVID-19 pandemic.
Conclusion
The overall ASD prevalence in children and adolescents in Korea seems to be increasing, especially in preschool children during the COVID-19 pandemic. Early and more effec-tive interventions are necessary for Korean children.
Introduction
For several decades, children presenting with developmental deviations in language and social and repetitive behaviors have been distinguished from children having other mental disorders and given a diagnosis of autism spectrum disorder (ASD) [1,2]. Most ASD patients will not live independently or work full-time [3]. Proper management strategies for preventing ASD should be applied, as well as suitable treatments for various ASD phenotypes. Recent genetic and molecular studies have discovered interesting patterns of risk factors, but without substantial practical implications [3-5]. To evaluate whether such strategies are valuable in a specific society, periodical analyses of the prevalence rate of ASD are essential.
Unfortunately, over the past decade, the prevalence of ASD diagnoses has in-creased considerably. A report from the United States focused on the prevalence and features of ASD among children aged 8 years in 2018 whose parents or guardians lived in 11 Autism and Developmental Disabilities Monitoring Network sites. The researchers found that 23 per 1,000 children (i.e., one in 44) aged 8 years had ASD and that the prevalence and median age of ASD identification varied widely across sites. These findings indicated a significant increase in ASD prevalence compared to 2014 (16.3 per 1,000). Furthermore, despite some small differences between regions, the prevalence of ASD was similar across racial groups in America. Potential reasons for the general increase in the prevalence of ASD include the extension of diagnostic criteria, the possibility of an earlier age at diagnosis age, better public awareness, or a mixture of factors; however, a consensus is yet to be reached [6]. Moreover, a significant economic burden is placed on children with ASD and their families, mainly due to the need to provide support to adults who cannot function independently, and this results in higher health-care expenses, increased child-care time, and loss of caregivers’ income [7]. Therefore, institutional and economic support is needed for people with ASD at the government level; to support such initiatives, it is important to periodically update the prevalence rate, especially among the pediatric population, as most ASD diagnoses occur during childhood.
According to earlier research using information from the Korean National Health Insurance Service (NHIS), the ASD prevalence was lower than the prevalence derived from questionnaire surveys [1]. However, using NHIS data to estimate the ASD prevalence may lead to an underestimate, considering that there are patients who have received alternative medical treatment or who cannot receive medical services. Although the accuracy of the diagnostic portion of NHIS data remains a matter of debate, we believe that the prevalence calculated using this data can be used to study changes in prevalence over time because the methods used for estimation are consistent. Estimating the prevalence rate using NHIS data avoids selection bias because the NHIS data are drawn from the entire population. This method also has the advantage of saving time, cost, and effort compared to conducting direct examinations or using a questionnaire [8].
To date, the ASD survey methodology has not been standardized. Existing studies all have unique designs that reflect the domestic social and health policies for children with disabilities [9]. This study provides up-to-date data on ASD prevalence in children and adolescents aged under 18 years in 2011 to 2021 from the NHIS, including the entire population living in the nation and presenting objective and reliable data [10].
Materials and Methods
1. Inclusion criteria
We performed this retrospective study using information from the NHIS in Korea. We used data on ASD (codes F84.0, F84.1, F84.5, F88.8, or F88.9 according to the International Classification of Diseases [ICD], 10th revision), as in a previous study, through the homepage of the NHIS (http://www.nhis.or.kr) that provides various information [11]. This information is based on insurance claims submitted by doctors after examining ASD patients from 2011 to 2021. The data are generated by clinics and hospitals that send diagnoses to the National Health Insurance Corporation after examining patients with a standard principal diagnosis. The medical departments associated with the data were pediatrics, psychiatry, rehabilitation medicine, and neurology. The number of patients with ASD was counted as those who received actual medical treatment each year. Those who visited medical clinics with a diagnosis of ASD more than once a year were counted as single patients in this study.
2. Sample collection and processing
We estimated the number of patients who met the conditions every year by calculating the number of people who visited clinics at least once a year for the treatment of ASD. Information on the age and sex of the aggregated patients was also obtained. From the homepage of Statistics Korea (http://www.kostat.go.kr), values for the estimated population of all age groups from 2011 to 2021 were collected.
3. Data extraction
The annual prevalence of ASD was derived by dividing the number of patients by the estimated population each year. We also calculated the prevalence of ASD by age and sex. Children and adolescents were stratified into three age groups (2–5, 6–12, and 13–18 years). Although ASD is sometimes diagnosed as early as the age of 18 to 24 months, the authors did not analyze those under the age of 2 [1,12].
Statistical values such as P values or confidence intervals were not needed, as this study evaluated the entire population of Korea, not randomly selected samples [8].
4. Ethics
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of Chuncheon Sacred Heart Hospital (CHUNCHEON 2022-01-015). Written informed consent by the patients was waived due to a retrospective nature of our study.
Results
Table 1 indicates the calculated prevalence rates of ASD in Korea by age (0 to 18 years) from 2011 through 2021. Each year, the highest prevalence appeared among 6 years old, and beyond this age, the prevalence decreased with age. Every year, boys had a higher prevalence than girls aged 2 to 18 years (median, 4.9 times higher; range, 2.7 to 7.6 times).
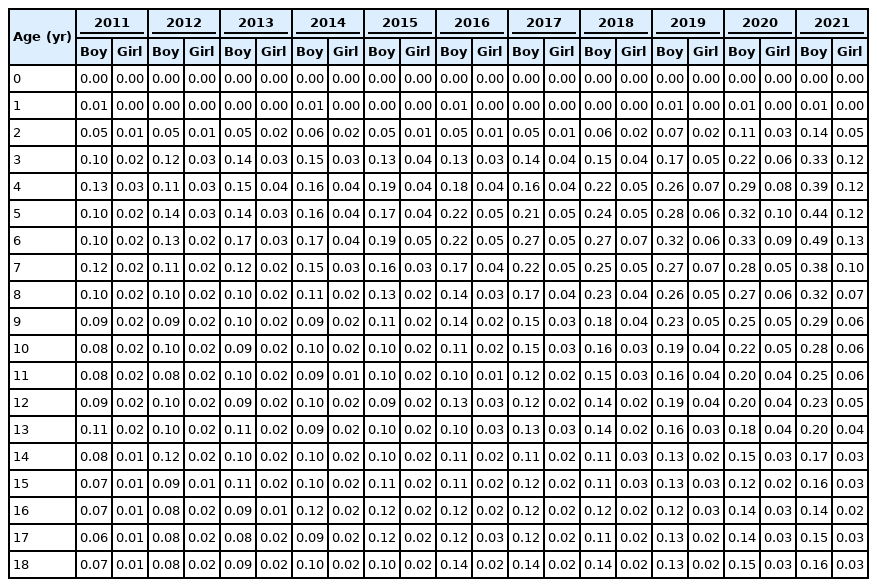
The estimated prevalence rate (%) of pediatric autism spectrum disorder in Korea from 2011 through 2021
Our analysis of time trends in prevalence based on age group showed that the prevalence of ASD in Korean children (2 to 18 years) increased markedly from 0.05% in 2011 to 0.17% in 2021 (Fig. 1). In particular, the ASD prevalence in preschool-aged children (2 to 5 years) increased from 0.06% in 2011 to 0.23% in 2021. Additionally, the prevalence in adolescents (13 to 18 years of age) increased from 0.05% in 2011 to 0.10% in 2021. Notably, ASD prevalence in every age group demonstrated a rapid in-crease during the coronavirus disease 2019 (COVID-19) pandemic (2020 to 2021). The prevalence was lower in preschool-aged children (2 to 5 years) than in children aged 6 to 12 years from 2017 to 2019 and higher thereafter, from 2020 onward (during the COVID-19 pandemic).
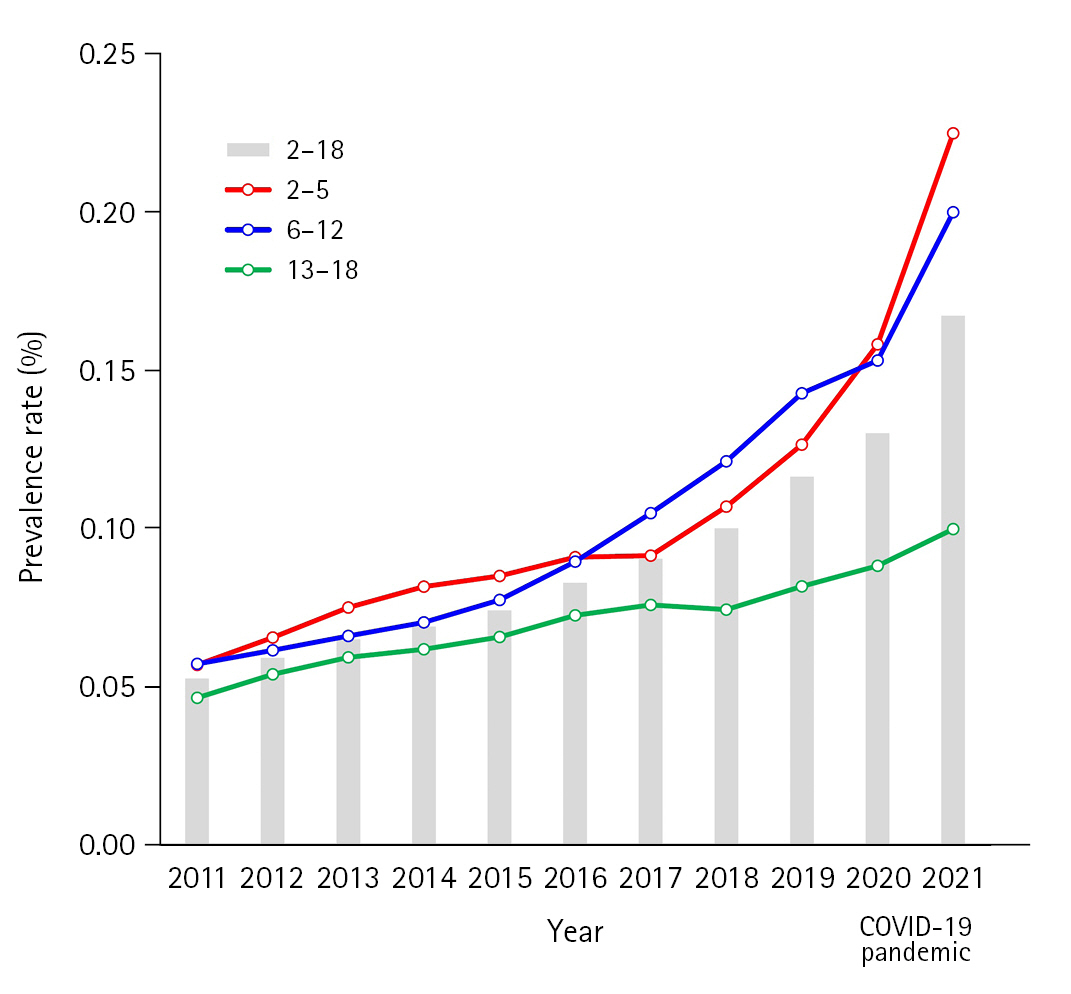
Time trends in the prevalence of autism spectrum disorder (ASD) in Korean children aged 18 years and under from 2011 to 2021. Changes in ASD prevalence in each age group from 2011 to 2021 were observed in the following age groups: overall (2–18), 2–5, 6–12, and 13–18 years. COVID-19, coronavirus disease 2019.
We analyzed whether the trend of increasing ASD prevalence with age was similar every year (Fig. 2). The prevalence rates for 2011, 2014, 2017, and 2021 were compared. In 2011, the highest prevalence rate by age group was 0.08%, but it increased to 0.31% in 2021. In 2021 (during the COVID-19 pandemic), the prevalence of ASD in children under the age of 10 increased significantly compared to the prevalence in 2011, 2014, and 2017. Remarkably, the prevalence of ASD in 6 years old increased five-fold, from 0.06% in 2011 to 0.31% in 2021.

Comparison of the prevalence of autism spectrum disorder (ASD) by age group among the years 2011, 2014, 2017, and 2021. The slope of ASD prevalence by age was different between the years. The prevalence of ASD in 2021 was much higher than in other years.
In addition, the slopes of increasing ASD prevalence were not the same according to age based on the year of birth (2011 to 2015) (Fig. 3). Among children who were born in 2011, 2012, and 2013, the increasing trend lines were similar. In contrast, in children born in 2014 and 2015, the slopes of prevalence increased more steeply as children grew, especially for those born in 2015.
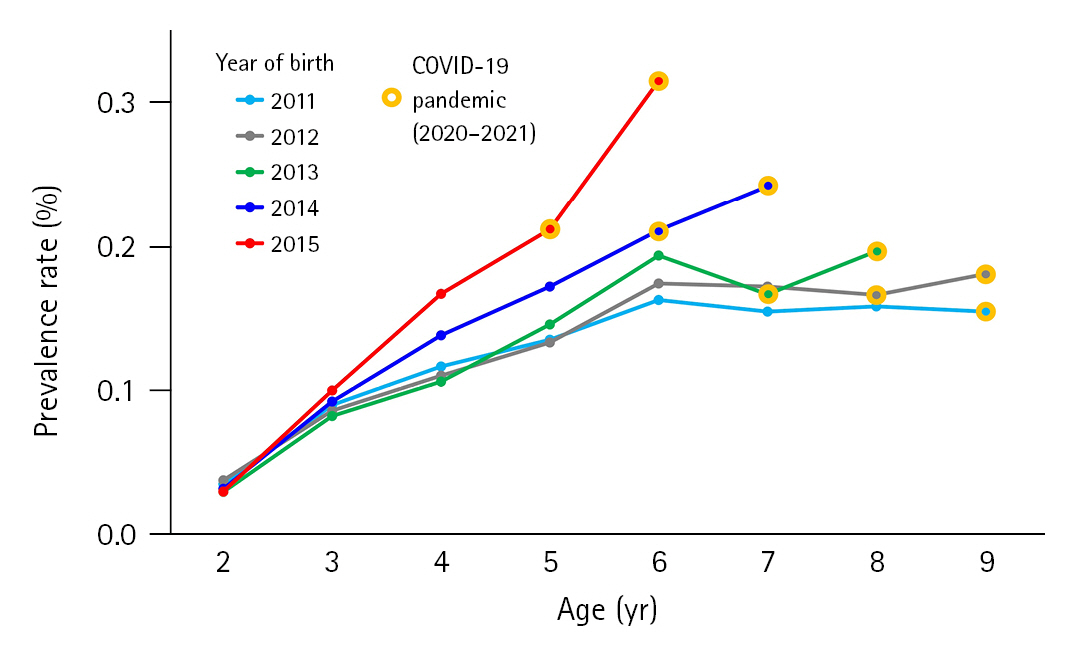
Comparison of the prevalence of autism spectrum disorder by age among children born from 2011 to 2015. Among children who were born in 2011, 2012, and 2013, the slopes of the increasing trend lines were similar. In contrast, in children born in 2014 and 2015, the slopes of prevalence with growth increased sharply. COVID-19, coronavirus disease 2019.
Discussion
The overall prevalence of ASD in children aged 2 to 18 years steadily increased from 2011 to 2021. Notably, the prevalence of ASD in preschool children (2 to 5 years of age) increased from 0.06% to 0.23% during the 11-year study period. The increasing prevalence of ASD in Korea is consistent with that of other developed countries [1]. We also compared prevalence rates by age group among children born in the years 2011 to 2015. We postulated that each group would eventually emerge from the disease at a similar rate, so that the difference in prevalence between groups would be maintained as the children grew. Interestingly during the COVID-19 pandemic (2020 to 2021) the slope of the prevalence of ASD between groups defined by birth year became larger with age. This indicates that the COVID-19 pandemic seemed to increase the incidence of ASD, especially in preschoolers.
Although the precise reason has not been definitively established, the increasing trend of ASD prevalence may be related to environmental changes and increased community awareness regarding the condition globally [1,3]. Countries that periodically investigate the prevalence of ASD include the United States, Canada, Korea, France, Australia, and Taiwan. In the United States and Canada, the prevalence rate is investigated every few years with data provided by community medical and educational service providers (United States surveyed about 220,000 people aged 8 years, and Canada surveyed about 40,000 people aged 1 to 17 years) [13-15]. France and Australia use national health registries (France surveyed about 300,000 people aged 7 years, and Australia surveyed about 5,000 people aged 6 to 7 years) [15,16]. Similarly, Taiwan used its disability registry data, surveying about 300,000 people aged 3 to 17 years each year between 2004 and 2010 [17,18]. As mentioned earlier, Korea uses the NHIS database for the entire nation. One study surveyed the prevalence rate with data from all children in Korea who were treated under the diagnosis of childhood autism from 2008 to 2015 [6].
According to a global estimate of ASD prevalence prepared using the results of those studies, the median prevalence in 2022 is 65/10,000, which is higher than the rate of 62/10,000 reported in 2012. Most of the studies reported in this study were performed in the United States and Europe, Western Pacific, and South-East Asia, and a few studies from Africa and the Middle East were also included [1]. It is already well-known that the main cause of ASD is genetics. A recent study examining the relationship between genetic and environmental factors and the incidence of ASD in five countries found that the heritability of ASD was about 80%, implying that ASD occurrence across the world is mostly due to genetic factors and that the impact of environ-mental factors is small [19]. Thus, the reason for the continuing increase in the global prevalence of ASD is thought to be due to “alteration in community awareness world-wide,” “broadened diagnostic boundaries over time,” “increased diagnosis of milder forms,” and “increased diagnosis in previously underdiagnosed populations” [1]. According to one of the latest Centers for Disease Control and Prevention reports estimating the prevalence of ASD in 2018, in which racial disparities reflected in ASD prevalence were monitored for many years, there was a slight difference in overall ASD prevalence in America among races, which were defined as including White (non-Hispanic) and Black (non-Hispanic), Hispanic, Asian/Pacific Islanders, and American Indian/Alaska Native children [14]. One study from Israel reported significantly lower rates of ASD prevalence among Arab and ultra-Orthodox populations [20].
The observed patterns in the changing prevalence rate according to age in Korea may be explained by opinions specific to Korean culture, such as “a feeling of rejection about seeing a psychiatrist” and “fear of being diagnosed with ASD or registration as a person with disabilities” [21]. Families need a medical certificate for a disabled child to attend a special school and for insurance coverage [22]. For this reason, the prevalence rate increases until 6 to 7 years, which is when children start school in Korea. However, difficulties continue even after an ASD diagnosis is made. First, there is a shortage of resources such as special schools, special classes in general schools, specialist teachers, and educational assistance, and to make matters worse, most of the resources are for patients with intellectual disabilities [23]. In Korea, 1.35% of all students receive special education, compared to 3% of all students in Japan [24]. Second, there is a lack of national support for treatment. In Korea, the developmental rehabilitation service provides KRW 220,000 (about 153 US dollar) worth of vouchers per month to children with brain lesions, blindness, hearing impairment, speech impairment, intellectual disability, and autism, which is far from adequate to cover the cost of treatment [22,25]. Third, there is a lack of professionals and no domestic training system for evidence-based interventions for ASD [10]. As the importance of early intervention is being increasingly studied and gaining more attention, this shortage of professionals should be improved as soon as possible [26,27].
A typical limitation of research using information from the NHIS is diagnostic accuracy. Furthermore, since the prevalence of ASD is estimated on the basis of patients’ hospital visits, it may be affected by factors like ability to access clinics, patients’ socio-economic status, disease perceptions, or behavioral changes according to external considerations such as the COVID-19 pandemic. In other words, some patients may not seek medical care even if ASD has developed or if ASD symptoms persist. For this reason, all analyses using the NHIS data should be interpreted carefully. In fact, a previous study reported a higher prevalence rate than our findings (2.64% of the total population in 7 to 12 years old between 2005 and 2009, n=55,266) [28]. This would appear to be a large difference from the prevalence rate among 6 to 12 years old in 2011 in our study (0.06%). This discrepancy seems to be due to the cumulative impact of the limitations of this study using the NHIS database, which only includes information from hospital visits, and differences in research methods, as the other study used a questionnaire among a relatively small population. National epidemiological studies using other research methods, such as clinical observation or parent interviews, are necessary to reach a more conclusive estimate of the ASD prevalence in the Korean pediatric population. Since this study collected patient information based on diagnostic codes, the accuracy of these codes is important, and in Korea, the Korea Standard Disease Classification (KCD), which is being revised by applying the World Health Organization's ICD code changes, is used and revised periodically. The ASD-related KCD diagnostic codes did not change during our study period. Thus, our methods obtained consistent and comparative data. Additional well-constructed cohort studies to validate these trends and to discover factors affecting the epidemiology of ASD are necessary.
Clearly, national epidemiological studies using a different approach are necessary to determine the trends in ASD prevalence in Korean children. During the COVID-19 pandemic, hospital visits generally decreased significantly (Organization for Economic Co-operation and Development statistics on doctor consultations). Nevertheless, the prevalence of ASD in 2020 to 2021 markedly increased. As an explanation for the increased prevalence of ASD during the COVID-19 pandemic, we suggest that measures like mask-wearing during the COVID-19 pandemic might have interfered with children’s development, especially language development, in which children learn by looking at their caregivers’ mouths and facial expressions [29,30]. Due to self-isolation and social distancing to prevent the spread of infection, professional education hours have decreased in daycare centers, and children with ASD symptoms have experienced an aggravation of psychiatric and behavioral problems [31,32]. Another possibility for the increased prevalence of ASD may be that medical visits for ASD have increased because families have spent more time at home during the COVID-19 pandemic, making parents more likely to perceive abnormal behavior.
In conclusion, we first estimated the prevalence of ASD by year based on the Korean NHIS database and observed temporal trends over the past 10 years, including the COVID-19 pandemic. The overall prevalence of ASD in Korean children aged 2 to 18 years increased from 2011 to 2021, especially in 2 to 5 years old during the COVID-19 pandemic. In contrast, the prevalence of ASD in adolescents (13 to 18 years old) tended to increase slightly during the same period. Our results suggest that strategies need to be modified for timelier and more effective prevention and care of ASD in Korean children.
Notes
No potential conflict of interest relevant to this article was reported.
Author contribution
Conceptualization: JY and JYL. Data curation: HE. Formal analysis: HE. Methodology: MK. Writing-original draft: HE. Writing-review & editing: MK, JKY, EB, JY, and JYL.
