Reversible Cerebral Vasoconstriction Syndrome Presenting with Thunderclap Headache in a Child
Article information
Reversible cerebral vasoconstriction syndrome (RCVS) is a clinical and radiological diagnosis characterized by the acute onset of headache, multiple constrictions of several cerebral blood vessels, and remission within 3 months [1]. Thunderclap headache, which usually lasts for 1 to 3 hours, is a typical symptom accompanying RCVS, and focal neurologic deficits may also occur due to hemorrhages, infarcts, and even posterior reversible encephalopathy syndrome (PRES) [2]. RCVS predominantly occurs in middle-aged women aged 30 to 50 years [1]. Only small case series and individual cases of RCVS have been reported in children [2]. We describe a healthy child with a thunderclap headache associated with RCVS, which is the first pediatric case of this condition in Korea.
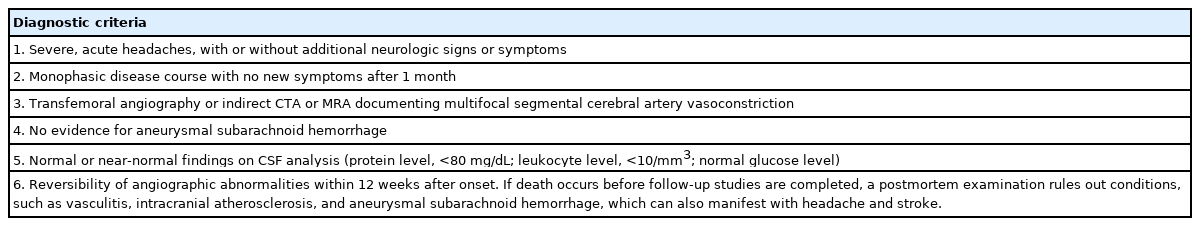
An 8-year-old boy presenting with sudden-onset, severe, and diffuse headache was referred to our pediatric neurology clinic. He described thunderclap headaches with a verbal numeric pain scale of 9 to 10 intensity within 2 hours of falling asleep. He woke up with a severe headache, and taking acetaminophen did not help. The patient was born full-term without any perinatal problems, and his medical history was unremarkable. He and his family had no history of headaches, migraines, or neurological diseases. He was not taking any medications. On admission, his neurological examination results were normal. His blood pressure was 110/70 mm Hg. A complete blood count, serum electrolyte concentrations, serum glucose level, hepatic and renal function tests, thyroid function test, and routine urinalysis all showed normal results. Brain magnetic resonance imaging (MRI) and magnetic resonance angiography (MRA) showed multiple segmental narrowing of the cerebral arteries without brain parenchymal lesions (Fig. 1A); however, electroencephalography showed normal findings without focal slow waves.
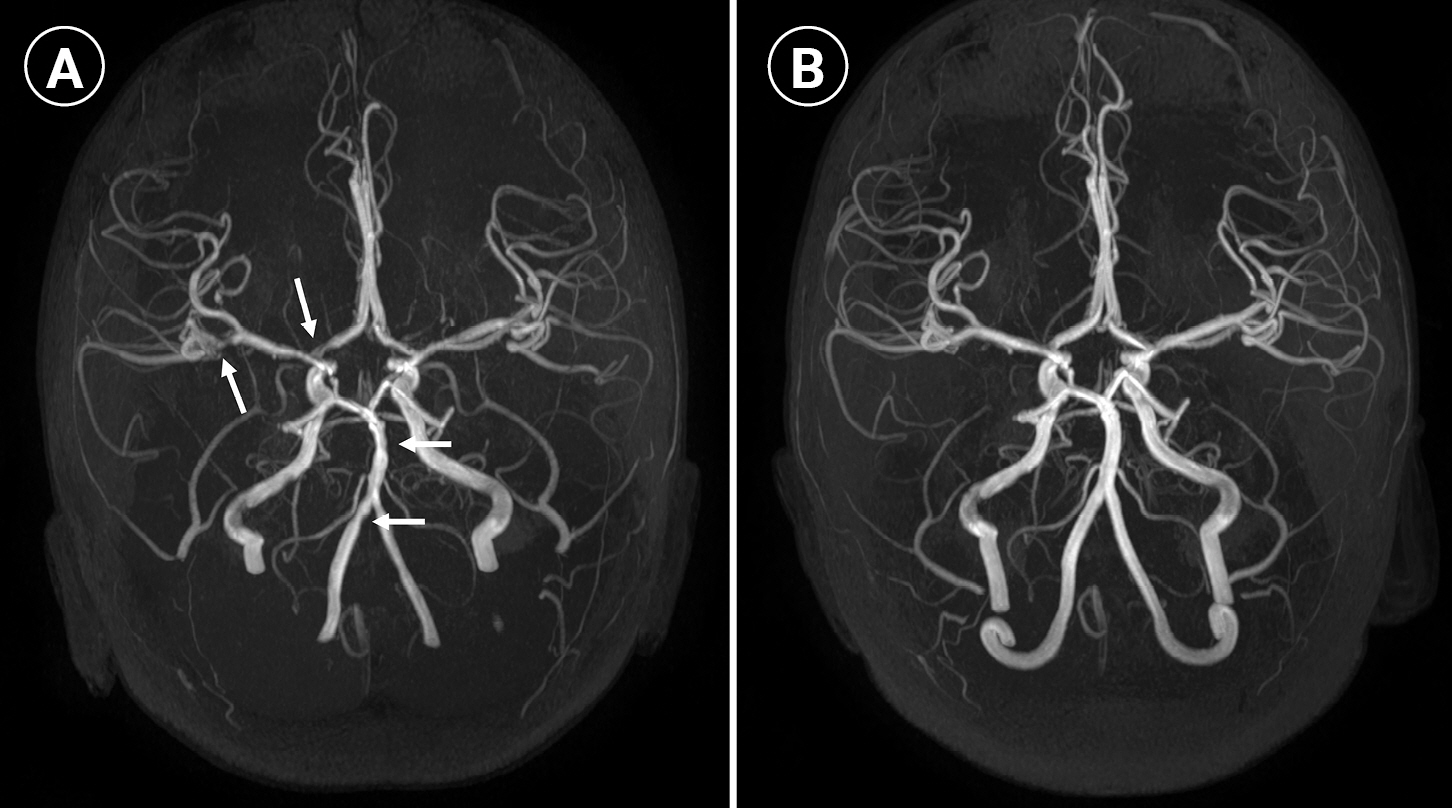
(A) Magnetic resonance angiography (MRA) of the brain showing diffuse irregularity and beading appearance of bilateral vertebral arteries, basilar artery, bilateral middle cerebral arteries, and the right anterior cerebral artery (arrows). (B) Follow-up MRA after 2 months showing normal caliber and reversal of vascular abnormalities.
Several laboratory tests were performed under the suspicion of arteriopathy or an infectious or rheumatologic disorder. The erythrocyte sedimentation rate and C-reactive protein level were normal. Cerebrospinal fluid (CSF) analysis revealed a normal cell count (0/μL), protein level (21 mg/dL), and glucose level (72 mg/dL), with a normal opening pressure (17 cmH2O). The CSF bacterial culture was negative, and polymerase chain reaction tests did not detect herpes simplex virus, human herpes virus 6, varicella zoster virus, or enterovirus. The plasma von Willebrand factor antigen test, performed to detect primary angiitis of the central nervous system, was normal. He had normal procoagulant screening results, including protein C, protein S, antithrombin III, homocysteine levels, negative lupus anticoagulant, and cardiolipin antibodies. His autoimmune workup, including rheumatoid factor, antinuclear antibodies, complement levels, antiphospholipid antibodies, and anti-neutrophilic cytoplasmic antibodies, also showed normal results. An electrocardiogram and echocardiography showed normal findings.
Pediatric RCVS was suspected, and he was started on 5 mg of flunarizine. His headaches improved. Repeated MRA 2 months later showed complete resolution of these areas of stenosis (Fig. 1B). Flunarizine was discontinued. He remained asymptomatic 1 year later, with no further headaches.
The requirement for written informed consent was waived due to the retrospective nature of the study, and the research was approved by the Institutional Review Board of Inje University Busan Paik Hospital (Busan, Korea; approval number: 2022-03-010).
RCVS is characterized by a thunderclap headache with or without neurological deficits, normal or near-normal CSF analysis, cerebral artery stenosis, or multifocal segmental areas of vasoconstriction, which generally resolve within a few weeks [3]. Calabrese et al. [4] proposed diagnostic criteria for RCVS in 2007 that were slightly modified by the International Headache Society (Table 1) [1]. These criteria are useful for diagnosing RCVS and increasing physicians’ awareness of this disease. Our patient met all these criteria and was diagnosed with RCVS.
RCVS has been well-studied in adult patients. A large adult case series showed that RCVS commonly affects middle-aged women [5,6]. In contrast, a review of pediatric RCVS patients reported a male predominance [2,7]. Brain computed tomographic angiography or MRA is useful for diagnosing RCVS. However, signs of vasoconstriction can be noticed 7 to 14 days after the onset of the headache [2,7]. Headache can precede the onset of brain angiography findings showing vasoconstriction, which causes difficulties in accurate diagnosis [2]. Therefore, repeat imaging after 1 to 2 weeks is necessary to confirm the diagnosis in patients with recurrent severe headaches [2,8]. Additionally, CSF analysis and blood laboratory tests must be performed to rule out infection or inflammation.
However, the pathogenesis of RCVS remains unknown. The most important hypothesis is an alteration in the autonomic regulation of cerebral vascular tone, which leads to multifocal narrowing of the cerebral arteries and severe headache [1,2]. Another proposed mechanism is increased leakage of the blood-brain barrier caused by the disruption of arterial tone; this has been postulated as a hypothesis for PRES, which is present in 25% of pediatric RCVS patients [2]. Stress or emotional changes that increase endogenous catecholamine release are also thought to be related to the development of RCVS [2].
The most important treatment for RCVS is supportive care such as hydration, bed rest, analgesics, blood pressure control, and avoiding triggering factors [7]. Calcium channel blockers are the most commonly used medications for vasodilation in the acute phase of RCVS [7]. Our patient was treated with flunarizine, a calcium channel antagonist, which showed good efficacy in controlling headaches. The recommended duration of oral medication is typically 2 to 3 months [7]. Some experts suggest that supportive care without pharmacotherapy, such as calcium channel blockers, may be sufficient to manage RCVS, because most patients generally have a benign clinical course without neurological complications [7]. More than 90% of patients with RCVS have a favorable prognosis, with a monophasic pattern [2,7]. However, major neurological complications, including stroke, intracranial hemorrhage, and PRES, can occur, particularly in patients with specific comorbidities, such as hemolytic uremic syndrome, systemic lupus erythematosus, and sickle cell disease [2,7]. Therefore, close monitoring and follow-up are necessary in pediatric patients with RCVS associated with hematologic or rheumatologic diseases.
In conclusion, this case report describes the first case of a healthy Korean child with RCVS. Although pediatric patients with RCVS have rarely been reported, RCVS can occur in children and adolescents. Brain MRI and MRA should be performed for children with severe and recurrent thunderclap headaches, the most common symptom in RCVS. Additionally, MRA can be a useful diagnostic tool in pediatric patients with thunderclap headaches and focal neurologic deficits such as sensory changes and a decrease in muscle strength and motor tone. Serial neuroimaging may be needed because initial imaging can show normal findings in patients with RCVS within 1 to 2 weeks of headache onset. Most patients with RCVS have a good prognosis, but clinical follow-up is necessary in consideration of neurological complications.
Notes
No potential conflict of interest relevant to this article was reported.
Author contribution
Conceptualization: BLL. Data curation: BLL. Methodology: BLL. Project administration: BLL. Visualization: BLL. Writing-original draft: BLL. Writing-review & editing: BLL.