Is Electroencephalography Useful in Children with Developmental Delays but without Overt Seizures?
Article information
Abstract
Purpose
Electroencephalography (EEG) is useful for clarifying the association between cortical activity and cognitive processes in children. We investigated whether EEG abnormalities were correlated with developmental delay/intellectual disability (DD/ID) in the absence of clinical seizures.
Methods
We retrospectively identified 166 children with DD/ID who underwent EEG at Pusan National University Hospital between January 2011 and December 2021. We compared clinical characteristics and test results between those with normal and those with abnormal EEGs. Additionally, we analyzed EEG abnormalities in relation to neurodevelopmental disorders, specifically autism spectrum disorder (ASD) and attention deficit hyperactivity disorder (ADHD).
Results
Of the 166 patients, 39 (23.5%) displayed abnormal EEGs, while 127 (76.5%) had normal EEGs. Of the former, 25 (64.1%) patients exhibited epileptiform discharges, including 22 (56.3%) with focal and three (7.7%) with generalized discharges. Focal discharges most frequently affected the central area (35.9%). Twenty patients (51.3%) exhibited rhythmic slowing patterns. Epilepsy diagnoses were significantly more common among patients with abnormal EEGs (n=8, 20.5%) than among those with normal EEGs (n=9, 7.1%) (P<0.001). Of 22 patients with ASD, five (12.8%) had abnormal EEGs. Of 13 patients with ADHD, five (36.4%) had abnormal EEGs, all with epileptiform discharges. Two patients with ASD and two with ADHD exhibited rhythmic slowing. Abnormal EEG findings were significantly more common among those with genetic abnormalities compared to genetically normal patients (26 vs. 13, P=0.017).
Conclusion
EEG represents a potential screening tool for children with DD. Abnormal EEG findings are associated with increased epilepsy risk, informing diagnosis and treatment planning.
Introduction
Human development, which refers to the transformation of a dependent infant into a self-sufficient adult, is a critical component of pediatric health. This process is typically categorized into several domains, including language, gross and fine motor skills, cognition, social and personal development, and activities of daily living [1]. Developmental delay (DD) is frequently identified in early childhood. DD can manifest as a lag in one domain, known as specific DD, or across multiple domains, termed global DD, both of which involve atypical progression [1,2]. Intellectual disability (ID) is more commonly diagnosed in children over the age of 5 years, when assessments of learning capabilities are more reliable [1]. The causes of DD/ID are diverse and can include genetic factors, complications during pregnancy or childbirth, and premature birth [3]. Early detection and intervention are crucial for improving outcomes in children with DD/ID, regardless of the underlying cause. DD is a common manifestation of various neurodevelopmental conditions, particularly autism spectrum disorder (ASD) and attention deficit hyperactivity disorder (ADHD). ASD is a complex neurodevelopmental disorder characterized by persistent difficulties in social communication and interaction, coupled with restricted and repetitive behaviors, interests, and activities [4]. These symptoms typically become clinically apparent in the early stages of development and can lead to varying degrees of impairment in individual, social, and occupational functioning, depending on the range and severity of symptoms. ADHD is a widespread neurobehavioral disorder marked by levels of inattention and hyperactivity that exceed what is expected for a child’s developmental stage [5].
Electroencephalography (EEG) is a technique for measuring the electrical activity of large groups of neurons firing synchronously, using electrodes placed on the scalp. This non-invasive test is valuable for studying the pathophysiology of brain diseases, including epilepsy, Alzheimer disease, and autism [6]. However, the impact of EEG discharges on cognitive and behavioral development remains unclear. Epileptiform discharges are frequently observed in various neurodevelopmental disorders, even in the absence of overt seizures [6-8]. The question of whether interictal epileptiform discharges—spikes or spike-wave complexes occurring without observed clinical seizures—are detrimental to cognitive development is a matter of debate [8]. Research has indicated that frequent epileptiform discharges, particularly in young children, may disrupt the development and function of neural networks [8,9]. Furthermore, EEG abnormalities are commonly found in patients with ASD and ADHD [10,11]. Considerable interest has been paid to the potential for early detection and intervention with EEG to improve health outcomes for children with DD [12].
Few studies have directly assessed the role of EEG in Korean children with DD/ID who do not have epilepsy. Therefore, this study was conducted to evaluate electrocortical profiles among children with DD/ID and to establish the clinical utility of EEG in this population, with a focus on ASD and ADHD.
Materials and Methods
1. Patients
We conducted a retrospective chart review of patients aged 0 to 18 years who presented for their first visit to Pusan National University Hospital between January 2011 and December 2021 and were diagnosed with DD/ID of unknown etiology. A total of 166 patients who underwent EEG without clinical seizures were included in the study. Global DD was diagnosed in children under 5 years old who exhibited delays in two or more of the following five domains: gross motor, fine motor, social and personal, language, and cognitive development. Initial screening was conducted using the Korean Ages and Stages Questionnaire or the Korean Developmental Screening Test for Infants and Children, with the Bayley Scales of Infant and Toddler Development, Third Edition, additionally used for DD diagnosis. ID was defined as an intelligence quotient score below 70 at 5 years of age or older, as measured by the Korean Wechsler Intelligence Scale [13]. The diagnostic criteria for ASD and ADHD from the Diagnostic and Statistical Manual of Mental Disorders, Fourth and Fifth Editions (DSM-4,5), were utilized for assessment [1]. For patients older than 12 months, additional symptoms indicative of ASD include reduced eye contact, lack of response to one’s name, altered behaviors related to shared interests (such as joint attention), severe language delays, lack of interest in peers, and deficits in imaginative and cooperative play. Children displaying these behaviors were recommended for further evaluation or referral to a child psychiatrist. In patients of school age or older, an ADHD diagnosis was considered if related symptoms were present. If ASD and ADHD were not diagnosed at the initial visit due to the patient’s young age or mild symptoms, a diagnosis was confirmed upon later suspicion through further evaluation during follow-up. The inclusion criteria were: (1) a diagnosis of DD/ID in a patient under 18 years of age; (2) a minimum follow-up period of 6 months; (3) the absence of overt seizures; and (4) the use of EEG for DD/ID assessment. The exclusion criteria were: (1) the performance of EEG following a clear seizure event; and (2) a previous diagnosis of epilepsy. Epilepsy was diagnosed based on the occurrence of two or more episodes of unprovoked seizures at least 24 hours apart. Medical records were retrospectively reviewed, and data were collected on demographic variables and birth history, with particular attention paid to prematurity and perinatal complications. Dysmorphic facial features, major or minor congenital anomalies, and clinical characteristics of the delay were noted. Reviews were conducted of metabolic/biochemical investigations, laboratory test results, neuroimaging findings, and genetic test outcomes. Metabolic/biochemical investigations included tandem mass spectrometry, thyroid function tests, and measurements of serum lactic acid/pyruvic acid, serum amino acid, ammonia, creatine kinase, urine glycosaminoglycan, and urine organic acid levels. Magnetic resonance imaging (MRI) findings were divided into six groups [14]: (1) normal; (2) non-specific findings, such as cavum septum pellucidum, cavum vergae, ventriculomegaly, enlarged subarachnoid spaces, hypoplasia of the corpus callosum, and delayed myelination; (3) congenital and developmental brain; (4) recognizable syndromes, including neurofibromatosis, tuberous sclerosis, and Sturge-Weber syndrome; (5) neurovascular diseases and trauma, such as hypoxic-ischemic injury or encephalopathy, periventricular leukomalacia, encephalomalacia, atrophy, and gliosis; and (6) metabolic and neurodegenerative diseases, such as demyelination. For patients with an undiagnosed condition, we performed chromosomal microarray analysis (CMA), karyotype analysis, and fragile X messenger ribonucleoprotein 1 (FMR1) gene testing for fragile X syndrome. If a specific disease was suspected based on the phenotype, targeted genetic testing was conducted, including tests for the methyl-CpG binding protein 2 (MECP2), dystrophia myotonica protein kinase (DMPK), survival motor neuron 1/2 (SMN1/2), and nuclear receptor binding SET domain protein 1 (NSD1) genes, as well as methylation polymerase chain reaction for Prader-Willi/Angelman syndrome.
2. EEG
EEGs were recorded using a brain monitor (Natus Medical Inc., San Carlos, CA, USA) equipped with a high-cut filter set at 70 Hz, for a duration exceeding 30 minutes during both sleep and alert states. This was accompanied by simultaneous video recordings and a single electrocardiogram channel. The EEG results used in this study were derived from the initial EEG conducted for each patient at our hospital. The number of subsequent EEGs varied among patients. Two experienced EEG technicians performed the EEGs, and three pediatric neurologists reviewed the recordings. Electrodes were placed in accordance with the international 10 to 20 system and referenced to both ears. For patients who were uncooperative, sedation was achieved using chloral hydrate. Abnormal findings were categorized into three groups: epileptiform abnormalities (including spikes, sharp waves, spike and wave discharges, polyspike and wave discharges, and hypsarrhythmia with either focal or generalized distribution), slowing abnormalities (with either focal or generalized distribution), and abnormal background activity (characterized by abnormal background frequencies with either focal or generalized distribution). Based on the findings, we classified patients into those with normal EEGs and those with abnormal EEGs.
3. Statistical analysis
Statistical analyses were performed using SPSS version 27.0 (IBM Corp, Armonk, NY, USA). Descriptive statistics are presented as means and standard deviations, continuous variables as means and ranges, and categorical variables as counts and percentages. To evaluate the significance of differences among the continuous and categorical dependent variables, a two-tailed chi-square test and an independent-samples t-test were employed. A P value of less than 0.05 was considered to indicate statistical significance. Multiple analysis of covariance (MANOVA), employed in the context of between-subject comparisons of variables, was utilized to examine the association between abnormal EEG findings and a combination of dependent variables, including ASD, ADHD, epilepsy, birth history, perinatal complications, MRI abnormalities, and genetic abnormalities.
4. Ethics
This study protocol was approved by the Institutional Review Board of Pusan National University Hospital (2304-008-125). Informed consent was waived due to the retrospective nature of the study.
Results
1. Demographic and clinical features
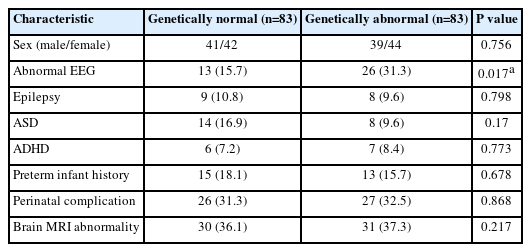
Overall, 179 patients were diagnosed with DD/ID and had undergone EEG. However, six patients were excluded because their EEGs were performed to evaluate seizures, not DD/ID. Of the remaining 173 patients, four were excluded because their DD/ID was confirmed following a seizure, and three were removed due to loss of data at follow-up. Ultimately, 166 children were included in this study (Fig. 1). Table 1 presents the demographic characteristics of the participants. Girls (51.8%) slightly outnumbered boys (48.2%). The age at presentation ranged from 1 month to 16 years, with a mean age (±standard deviation) of 2.8±3.16 years. The age distribution of patients was as follows: 56 infants (0−1 year old; 33.7%), 27 toddlers (1–2 years old; 16.3%), 58 preschoolers (2–5 years old; 34.9%), 18 patients who were 5–10 years old (10.8%), five who were 10–15 years old (3%), and two who were over 15 years old (1.2%). Regarding birth history, 28 patients (16.9%) were born preterm, and 53 patients (31.9%) had experienced perinatal problems such as respiratory distress syndrome, persistent pulmonary hypertension of the newborn, or congenital heart disease, necessitating neonatal intensive care unit admission. All patients underwent brain MRI; 105 patients (63.3%) displayed normal results, while 61 patients (36.7%) had abnormal findings, including corpus callosum hypoplasia/agenesis, periventricular leukomalacia, hypoxic brain injury, and intracerebral hemorrhage. During the follow-up period, comorbidity with ASD was observed in 22 patients (13.3%), whereas comorbidity with ADHD was observed in 13 patients (7.8%). The mean age at first diagnosis of ASD was 4.1±3.36 years, and the mean age at diagnosis of ADHD was 7.6±4.35 years. Patients not diagnosed with ASD or ADHD at the initial outpatient visit due to young age or mild presentation were tested and diagnosed in response to symptoms during the follow-up period. Seventeen patients (10.2%) were co-diagnosed with epilepsy. EEGs were performed for DD/ID evaluation in all patients without overt seizures; 127 patients (76.5%) had normal results, while 39 (23.5%) showed abnormalities. Epileptiform discharges were confirmed in 25 patients (64.1% of those with abnormal EEGs). MANOVA revealed relationships between abnormal EEG and epilepsy, perinatal complication, and brain MRI abnormality (P=0.015, P=0.029, and P=0.023, respectively). EEGs also revealed rhythmic slowing in 20 patients (51.3%) and other findings, such as bilateral EEG asymmetry, in three patients (7.7%).

Flow chart for patient selection. DD, developmental delay; ID, intellectual disability; EEG, electroencephalography.
2. Comparison between normal and abnormal EEG groups
Table 1 presents a comparison between the groups categorized based on EEG results. Of the patients with ASD, 17 individuals (13.8%) had normal EEGs, while five (12.8%) exhibited abnormal EEGs. Among patients with ADHD, eight (6.3%) had normal EEGs, and five (12.8%) had abnormal EEG findings. A significantly larger percentage of patients with DD/ID and abnormal EEG were later diagnosed with epilepsy (n=8, 20.5%) compared to those with normal EEG (n=9, 7.1%) (P=0.0016). Levels of ammonia and creatine kinase were significantly elevated in the abnormal EEG group compared to the patients with normal EEG (P=0.025 and P=0.024, respectively). Additionally, a higher proportion of patients with abnormal brain MRI findings was observed in the abnormal EEG group (n=20, 51.3%) compared to the normal group (n=41, 32.3%) (P=0.048). MANOVA revealed significant relationships between abnormal EEG and several factors, specifically epilepsy, perinatal complications, and abnormal brain MRI findings (P=0.015, P=0.029, and P=0.023, respectively).
3. Characteristic abnormal findings on EEG
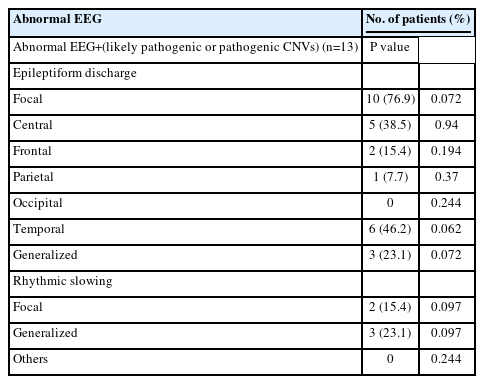
Table 2 presents the abnormal EEG findings from this study. Of the patients with abnormal EEG results, 25 (64.1%) exhibited epileptiform discharges, 22 (56.3%) showed focal discharges, and three (7.7%) displayed generalized discharges. Focal discharges occurred most frequently in the central region (35.9%), followed by the temporal (28.2%), frontal (12.8%), and parietal areas (10.3%). Rhythmic slowing patterns were observed in 18 patients (51.3%); with focal slowing—most commonly seen in the posterior head, including the occipital region—present in 11 patients (28.2%). Generalized slowing was noted in nine patients (23.1%). Among the patients with abnormal EEG results, four with ASD and five with ADHD exhibited epileptiform discharges. The EEG findings also revealed rhythmic slowing in two patients with ASD and two with ADHD.
4. Genetic test results
The patients underwent a series of genetic tests, with the results detailed in Tables 3-5. We compared the sex distribution between the patients with genetically normal findings and those with abnormalities, finding 41 boys in the former group (41/83, 49.4%) and 39 in the latter (39/83, 47%). The number of epilepsy diagnoses was comparable across groups, with nine patients in the normal group and eight in the abnormal group. Additionally, we examined comorbid diagnoses of ADHD (genetically normal, six patients; abnormal, seven patients) and ASD (normal, 14 patients; abnormal, eight patients); however, these differences were not statistically significant. Furthermore, no significant differences were observed between groups in terms of the number of patients with a history of preterm birth (15 vs. 13 patients, respectively), perinatal complications (26 vs. 27 patients), or brain MRI abnormalities (30 vs. 31 patients). However, the number of patients with abnormal EEG findings was significantly higher among the patients with genetic abnormalities (26 patients) compared to those with normal genetic findings (13 patients) (P=0.017) (Table 3).
In the group with abnormal EEGs, single gene mutation disorders were identified in five patients (12.8%). These included DMPK in two cases of congenital myotonic dystrophy, SMN1 in one case of spinal muscular atrophy type II, MECP2 in one case of Rett syndrome, and FMR1 in one case of fragile X syndrome. CMA revealed that 23 patients (59%) in the abnormal EEG group had various types of copy number variants (CNVs). A total of 39 CNVs were identified among these 23 patients. Twelve patients (30.8%) had one CNV each, eight patients (20.5%) had two CNVs each, two patients (5.2%) had three CNVs each, and one patient (2.6%) had five CNVs. Of these, 14 were microdeletions (35.9%) and 25 were microduplications (64.1%). In accordance with the American College of Medical Genetics and Genomics guidelines [15,16], the 39 CNVs were classified as follows: 11 were benign (28.2%), eight were likely benign (20.5%), five were variants of uncertain significance (VUS; 12.8%), one was likely pathogenic (2.6%), and 14 were pathogenic (35.9%). In the group with normal EEGs, 78 CNVs were identified: 25 benign (32.1%), 13 likely benign (16.7%), 12 VUS (15.4%), 11 likely pathogenic (14.1%), and 16 pathogenic (20.5%). Pathogenic results were significantly more common in the abnormal EEG group compared to those with normal EEG findings (P=0.033) (Table 4).
Pathogenic or likely pathogenic CNVs were considered positive CMA results. Among the group with abnormal EEG and positive CMA results, 10 patients (76.9%) exhibited focal epileptiform discharges, while three patients (23.1%) showed generalized discharges. The temporal area was the most common site for focal discharges, occurring in six patients (46.2%). Additionally, five patients (38.5%) demonstrated rhythmic slowing patterns, with focal slowing observed in two patients and generalized slowing in three patients. Our study did not reveal a statistically significant relationship between specific abnormal EEG findings and positive CMA results (Table 5).
The patients with abnormal EEG results were categorized into two groups: those with pathogenic/likely pathogenic CNVs (n=13, 30.8%) and those with nonpathogenic CNVs (n=26, 69.2%). Univariate analyses were employed to identify differences in various dependent variables among these patients based on CNV type. However, no statistically significant differences were found.
Discussion
Developmental disorders are common within pediatric populations [17]. EEG is the most accessible, informative, and cost-effective method for the evaluation and diagnosis of a variety of neurological diseases, and it is extensively utilized. However, EEG is not routinely recommended as a first-line diagnostic tool for DD/ID. Recent research has begun to highlight a potential relationship between DD and EEG findings [6,18]. Our study was designed to explore the association between EEG abnormalities and genetic anomalies in patients with DD/ID, with a focus on those with comorbid ASD or ADHD. In this retrospective analysis, we assessed 166 pediatric patients who met the DSM-4/5 criteria for DD/ID and had undergone EEG testing, despite having no history of overt seizures [1].
We reviewed and interpreted our study findings by addressing the following questions.
(1) Were any distinct clinical characteristics identified among the patients with abnormal EEG findings?
This study represented a comprehensive analysis of 166 pediatric patients diagnosed with DD/ID, focusing on EEG evaluations and subsequent clinical correlations. Notably, 39 individuals (23.5%) exhibited abnormal EEG results without overt seizures. These findings prompted an investigation into potential associations between EEG abnormalities and clinical characteristics within this cohort. Although no symptomatic seizures were observed before performing EEG, eight patients (20.5%) were diagnosed with epilepsy after experiencing seizures, a significantly higher proportion than in the group with normal EEG results (nine patients [7.1%], P=0.016). DD/ID and epilepsy are closely related, with increased rates of epilepsy observed in patients with DD. Numerous studies have reported a higher frequency of epilepsy co-occurring in children with neurodevelopmental disorders [19,20]. Additionally, individuals with neurodevelopmental conditions, such as ASD or ADHD and epilepsy, are more likely to display EEG abnormalities than their counterparts [21,22]. However, our understanding of patients with DD/ID and ASD or ADHD who display abnormal EEG results without experiencing seizures remains limited. This study provides valuable insights by demonstrating an elevated risk of subsequent epilepsy among patients with abnormal EEG findings and developmental abnormalities who have not experienced overt seizures. Laboratory findings revealed slightly high levels of ammonia and creatine kinase in the patients with abnormal EEG findings compared to the normal EEG group, although these levels remained within the normal range. Previous studies have confirmed meaningful temporary increases in creatine kinase and ammonia levels following clinical seizures [23,24]. However, since the patients in our study were tested without overt seizures, and their levels fell within a range that was normal and not pathologically high, these results are not expected to be clinically relevant. Approximately half of the patients in the abnormal EEG group exhibited abnormal brain MRI findings, a significantly higher proportion than in the normal EEG group. Previous MRI studies in children with DD/ID have reported widely varying rates of abnormalities [25-27]. Our findings align with several reviews, which included patients with concurrent neurological complications and reported MRI abnormality rates between 9% and 80%, with an average rate of 30% [25]. Among the MRI abnormalities identified in our study, mega cisterna magna, abnormal hippocampal shape, and choroid plexus cysts were considered minor abnormalities [28]. We believe these may be markers of brain dysgenesis. Other findings, which may lack clinical significance and have also been reported in typically developing children, include enlarged ventricles and prominent Virchow-Robin spaces [25]. Although classified as abnormalities here, these findings are unlikely to cause DD or affect EEG results (impacting five patients in the abnormal EEG group and six patients in the normal group, respectively). Excluding these individuals, the cross-analysis of the remaining patients with MRI abnormalities (35 patients in the normal EEG group and 15 patients in the abnormal group) revealed a value of P=0.205, indicating a lack of significance. However, many studies have reported associations between MRI abnormalities and DD/ID or seizures. Therefore, to obtain more definitive results, further follow-up evaluations of these children are warranted.
(2) Were specific abnormal EEG findings observed?
This study identified distinct abnormal EEG findings in the pediatric cohort evaluated for developmental disorders. The classification primarily involved epileptiform discharges and rhythmic slowing, which were further delineated by focal or generalized characteristics. Among the 39 patients with abnormal EEG results, the majority displayed focal or multifocal epileptiform discharges, with the central area representing the most common location. This was followed by the temporal, frontal, parietal, and occipital regions. Generalized discharges were relatively infrequent, observed in only three patients. Rhythmic slowing, noted in 18 patients, predominantly exhibited a focal pattern, with a minority displaying asynchronous EEGs. Notably, seven patients presented with both epileptiform discharges and rhythmic slowing. Furthermore, when examining specific diagnoses within the cohort, distinct EEG patterns emerged. Among patients diagnosed with ASD, epileptiform discharges were more prevalent (in four of five patients), whereas rhythmic slowing was observed in two cases. Conversely, all patients diagnosed with ADHD manifested epileptiform discharges, with two also displaying rhythmic slowing. These findings both align with and differ from previous studies on EEG patterns associated with ASD and ADHD. Other studies have reported paroxysmal slowing and epileptiform abnormalities in a significant proportion of EEG recordings in children with ASD [29]. In contrast, research on ADHD has highlighted increased absolute slow frequency activity, particularly of theta waves, and a decline in beta activity compared to typically developing children [30,31]. We emphasize the importance of clearly delineating EEG abnormalities in developmental disorders, as this could potentially provide insights into the underlying neural mechanisms and assist in enhancing diagnostic precision and guiding appropriate interventions for affected pediatric patients.
(3) What is the relationship between genetic confirmation and abnormal EEG findings? The etiology of DD/ID is highly diverse; however, this study demonstrates that causative genetic factors can often be identified through genetic studies [1]. Notably, one can observe a significant co-occurrence of DD/ID with other neurodevelopmental disorders, such as epilepsy, ASD, and ADHD [32-34]. This finding suggests that these neurodevelopmental disorders may share common biological mechanisms, implicating important biological pathways involved in neuronal development and function. Over the past few decades, interest has grown regarding genetic variations, leading to an increased understanding of the association between DD/ID and CNVs [35]. Consequently, CMA has recently emerged as the first-tier evaluation tool for the genetic diagnosis of DD/ID [3,17]. In this study, all patients underwent genetic studies, including CMA testing, as part of the evaluation for DD/ID. When comparing CMA results based on the presence or absence of abnormal EEG findings, we found that the rate of pathogenic findings was significantly higher in the group with abnormal EEGs (P=0.033) than in the group with normal EEG findings. This indicates that conducting additional EEG tests for children with DDs, where pathogenic CNVs have been identified through CMA, could be beneficial. Furthermore, we examined the relationship between cases categorized as “likely pathogenic” and “pathogenic” based on CMA results within the group with abnormal EEGs. Interestingly, a meaningful association between perinatal problems and abnormal EEG findings was observed, suggesting a statistical correlation between these factors and the presence of “likely pathogenic” or “pathogenic” CNVs.
(4) If an abnormal EEG finding is observed in a patient with DD/ID, is it appropriate to initiate interventions or treatments, such as anti-seizure medications (ASMs), even in the absence of overt seizures? In this study, we did not administer ASMs to patients with abnormal EEG findings because they exhibited no clinical seizures. ASMs were prescribed only when epilepsy was diagnosed in certain patients during the follow-up period. Research has long established that children with idiopathic DD/ID, with or without ASD and ADHD, exhibit a high rate of EEG abnormalities [36,37]. Over the past decade, a growing body of evidence has suggested a relationship of EEG findings with abnormal behavior and cognitive function. However, the risk-to-benefit ratio of using ASMs to reduce interictal epileptiform discharges is still unclear in most clinical contexts. Moreover, it remains inconclusive whether treating these abnormal EEG findings leads to improved patient outcomes [22,38,39]. Therefore, it is important to focus on active interventions that enhance patient outcomes rather than early initiation of ASMs. It is also essential to recognize that confirmed abnormal EEG findings, as seen in our study, may be associated with an increased risk of epilepsy.
This study had several limitations. First, its retrospective nature made long-term follow-up challenging. Second, the patient cohort was relatively small and consisted solely of outpatients from a single medical center. This limited sample size may have constrained the breadth of phenotype information and diminished the generalizability of the findings.
In conclusion, this study underscores the association between abnormal EEG findings, genetic anomalies, and DD/ID in pediatric patients, particularly those with co-occurring ASD or ADHD. Among 166 patients without seizures, those presenting with abnormal EEGs were found to have a higher likelihood of developing epilepsy later, exhibiting specific patterns such as epileptiform discharges and rhythmic slowing. Furthermore, our research highlights the potential clinical relevance of EEG abnormalities in guiding genetic evaluations for DD/ID. The findings addressed questions concerning the appropriate management of patients with DD/ID and abnormal EEG findings, particularly when seizures are not clinically evident. The link between abnormal EEGs and the subsequent onset of epilepsy in individuals with DD/ID emphasizes the need for vigilant monitoring and, where appropriate, targeted interventions.
Notes
Sang Ook Nam is an editorial board member of the journal, but he was not involved in the peer reviewer selection, evaluation, or decision process of this article. No other potential conflicts of interest relevant to this article were reported.
Author contribution
Conceptualization: YMK.
Data curation: YHJ.
Formal analysis: SHC.
Funding acquisition: HWY.
Methodology: HYJ and SJP.
Project administration: KHP and YMK.
Writing - original draft: YJL (Yoo Jung Lee) and YMK.
Writing - review & editing: JHK, YJL (Yun Jin Lee), SON, and YMK.
Acknowledgements
This work was supported by a 2-Year Research Grant of Pusan National University.