Pediatric cerebral and cerebellar infarctions are relatively rare, occurring at a rate of 1.6 per 100,000 annually [1,2]. The risk factors for pediatric stroke differ significantly from those in adults [1,3]. While cardiovascular diseases such as atherosclerosis are the primary causes of stroke in the elderly, non-atherosclerotic arteriopathy, infections, and genetic or metabolic disorders are more common causes in adolescents and children [1,3-5]. Interestingly, strenuous exercise and physical activity can trigger unusual cerebral vascular strokes in both adults and children [6-8]. This report presents a case of cerebellar stroke in a 9-year-old girl, which was induced by excessive crawl swimming.
A 9-year-old girl was admitted to the emergency department after experiencing sudden vertigo and nausea. These symptoms occurred following a 30-minute swimming lesson, her first in two years, during which she practiced the crawl stroke, kicked excessively, and inadvertently swallowed a significant amount of pool water. The patient exhibited severe vertigo, a tendency to lean to the right, difficulty walking, and muscle weakness in her right upper and left lower extremities. She also reported generalized muscle pain and a headache.
During a neurological examination conducted while the patient was standing upright, there was a noticeable tendency for the patient to lean to the right. This was observed alongside symptoms of nausea and vomiting, which occurred three times. Additionally, the patient struggled to walk in a straight line. Romberg's test results were negative, both with the patient's eyes open and closed.
The patient was alert and exhibited stable vital signs. Motor strength in the upper extremities was graded at IV/V, while the lower extremities were graded at V/IV. The finger-to-nose test showed sluggish responses, and ataxia was observed [9]. The patient was unable to walk in a straight line or stand without support. Upon performing the Dix-Hallpike test on the right side, the patient reported increased dizziness and headache compared to the left side [9]. Brain computed tomography showed no specific findings, and electrocardiography showed normal sinus rhythm with a heart rate of 88/min.
The patient was born prematurely at 34 weeks and subsequently required neonatal intensive care. Otherwise, she had been generally healthy with no known systemic diseases or vascular risk factors. Her laboratory values were consistently within normal ranges. This pediatric patient did not present any typical risk factors such as hypertension, dyslipidemia, or a history of smoking. Both her cardiac enzyme and lipid levels were within normal parameters, and her electrocardiogram showed no signs of arrhythmia, including atrial fibrillation, which is a common cause of cerebral infarction. There was no family history of stroke or cardiovascular disease. In terms of coagulopathy, her platelet count, platelet time, and activated partial thromboplastin time were all normal, measuring at 361,000/mm3, 12.7 seconds (international normalized ratio, 1.1) , and 32.6 seconds, respectively. Her D-dimer levels were also within the normal range, at less than 0.3 mg/dL. There were no physical examination findings or personal or family history suggestive of clotting disorders, such as petechiae, bruising, purpura, or recurrent nasal bleeding.
After receiving fluid treatment and resting in bed, the patient still experienced a right tilt the following day. However, her symptoms of vomiting, headache, and dizziness had significantly improved. On the 3rd day of hospitalization, the patient was able to stand upright without tilting, whether her eyes were open or closed. She was able to walk with the assistance of a guardian and a cane, and eventually began to walk slowly on her own.
Considering the possibility of peripheral vertigo-related disease, a vestibular function test was conducted, but the results were negative [5]. Once peripheral vertigo was definitively excluded, brain magnetic resonance imaging and magnetic resonance angiography were carried out.
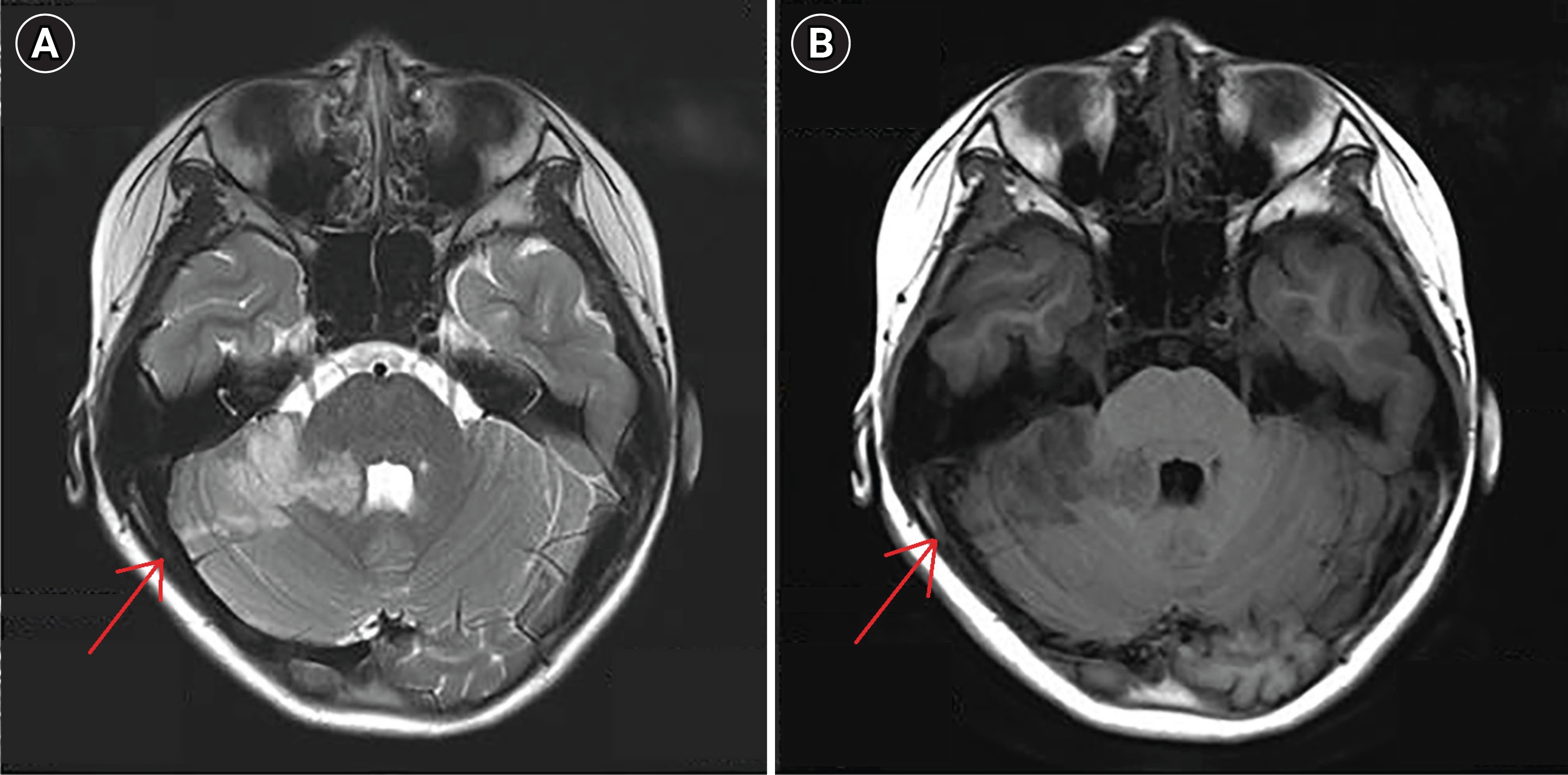
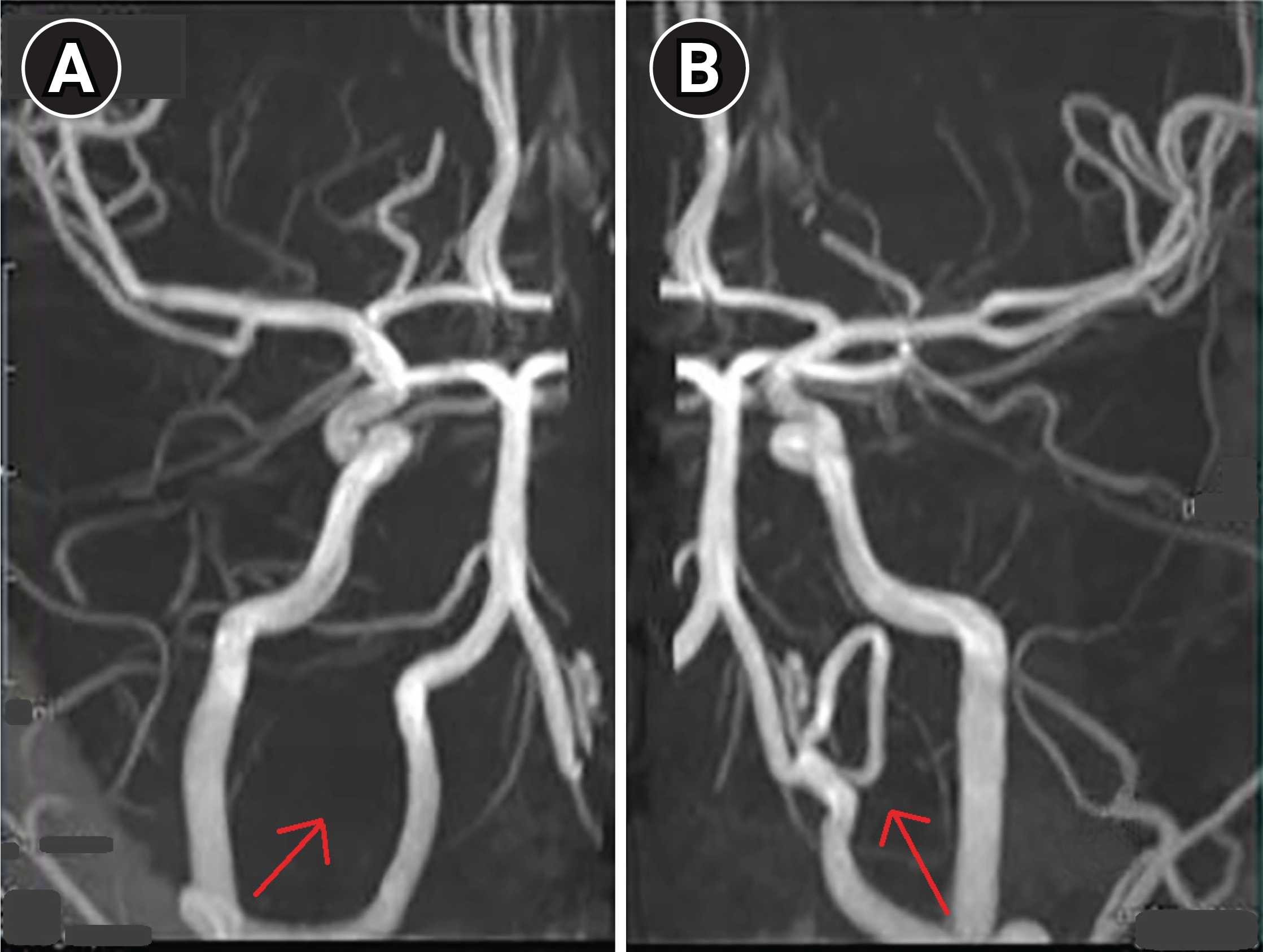
A sub-acute infarction, primarily in the territory of the right superior cerebellar artery, was suspected due to the presence of a high T2 signal in the right cerebellar hemisphere and right middle cerebellar peduncle (Fig. 1). The right posterior inferior cerebral artery was not visible, while the left was notably prominent, presumably providing blood supply to both posterior inferior cerebral artery territories (Fig. 2).
The patient began oral antiplatelet therapy with a daily dose of 100 mg of aspirin. She was then transferred to a tertiary care center for further assessment, with angiography being considered. After a week, the patient made a full recovery without the need for any additional interventions and has since been attending regular follow-up appointments.
Pediatric stroke is a heterogeneous condition in terms of its causes and symptoms [1,3]. Unlike adult stroke, which has a well-established and evidence-based treatment protocol, pediatric stroke presents a challenge due to delays in diagnosis [1,3-5,10]. The diversity of its causes and the variety of its presentations make it difficult to standardize treatment, leading to further delays in accurate diagnosis and management [1-3,10]. In adults, ischemic stroke is primarily caused by arterial blockage due to atherosclerotic plaque or thromboembolism [1,3,4]. However, in children, a range of underlying systemic conditions, including acute systemic disorders or non-atherosclerotic arteriopathies, complicate early-stage treatment [1-4].
Diagnostic imaging in this case highlighted the limitations of initial non-contrast computed tomography, which appeared normal despite the early stages of an ischemic stroke [5]. In adults, brain computed tomography serves as a valuable diagnostic tool, primarily used to rule out hemorrhagic stroke when an ischemic condition is strongly suspected [5,10]. However, in children, clinical presentations can vary greatly, often leading to an underestimation of the possibility of an ischemic stroke [1,10]. Current guidelines for pediatric stroke suggest magnetic resonance imaging as the preferred initial diagnostic imaging modality, with a recommended minimum protocol to reduce acquisition time [10]. In this particular case, any further delay caused by the scheduled magnetic resonance imaging acquisition could have potentially postponed the diagnosis.
The connection between sports and related injuries is well-documented, but the relationship between specific sports activities and stroke is not currently clear [6-8]. This relationship may be specific to the type of sport or the specific movements involved in certain activities [6-8]. In our patient's case, sudden repeated hyper-rotations of the neck may have resulted in a cerebellar infarct, similar to what has been reported in adults [6-8]. These reports suggest that impacts, collisions, or microtraumas related to sports activities can lead to subsequent strokes. Furthermore, certain sports, such as surfing, which involve hyperextensive maneuvers, may cause ischemic injuries [6-8]. Further studies are needed to understand the relationship between independent or repetitive maneuvers in sports activities and ischemic injuries, in order to prevent or early detect ischemic events.
This study was approved by the Institutional Review Board of Daejin Medical Foundation Bundang Jesaeng Hospital(approval number: DMC 2023-04-002). Written informed consent by the board was waived due to a retrospective nature of our study.