New Daily Persistent Headache after COVID-19 Vaccination in an Adolescent Patient
Article information
New daily persistent headache (NDPH), according to the International Classification of Headache Disorders-3 (ICHD-3), is a primary headache lasting >3 months for which patients remember the exact onset. Historical evidence supports the possibility of viral infections, including coronavirus disease 2019 (COVID-19), triggering a new onset of persistent headache [1]. A few cases of NDPH after COVID-19 have been documented in children and adults (Table 1) [2-4]. Similarly, although persistent headaches after vaccination against COVID-19 have been described, there is a paucity of literature on NDPH after COVID-19 vaccination [5,6]. Herein, we report a case of an adolescent patient diagnosed with NDPH after receiving a second dose of the BNT162b2 mRNA COVID-19 vaccine (Pfizer Inc., New York, NY, USA).
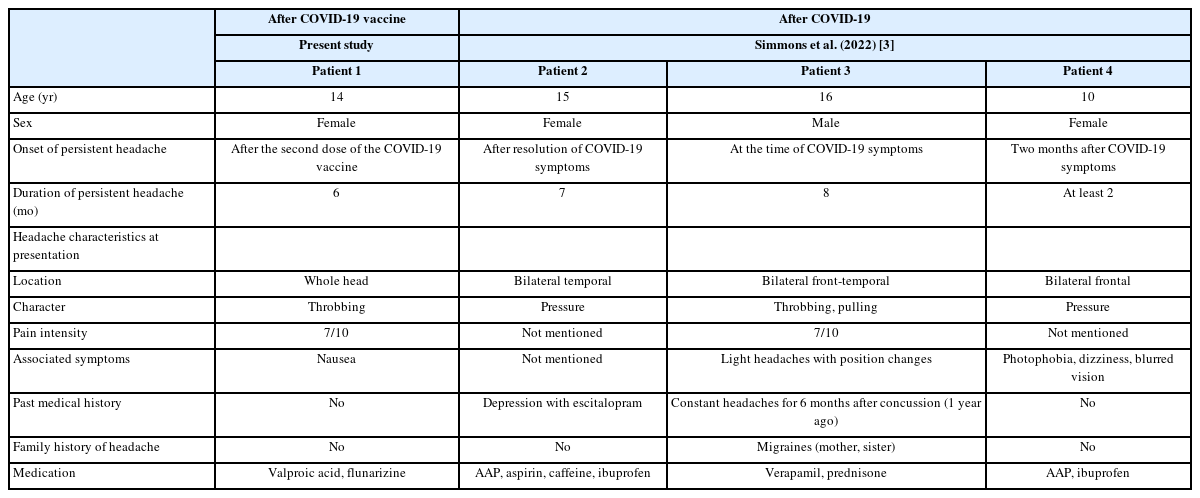
Pediatric cases of (probable) new daily persistent headache associated with COVID-19 and the COVID-19 vaccine
A previously healthy 14-year-old female soccer player visited Chungbuk National University Hospital because of persistent headaches that began 3 weeks prior to admission. The headaches began suddenly on the day the second dose of the BNT162b2 mRNA COVID-19 vaccine was received, and the patient described them as involving throbbing pain in the entire head. Continuous headaches persisted on a daily basis (numeric rating scale [NRS], 4/10). Severe headache attacks occurred four times per day (NRS, 7/10) and lasted from 30 minutes to 2 hours. The headaches were aggravated by movement, such as walking and riding in a vehicle. Severe and persistent headaches were progressive, interfered with daily activities, and did not improve with rescue drugs. The patient’s medical history revealed no previous head trauma, headaches, or neuropsychiatric conditions. There was no family history of primary or secondary headaches (Table 1).
During the first admission, which lasted 6 days, supportive care was provided with intravenous hydration and acetaminophen, as well as oral naproxen. No neurologic deficit was noted; however, the patient exhibited neck stiffness. No abnormal laboratory findings, including platelet counts and coagulation profiles, were noted. Antibody tests against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) were positive for the spike (S) protein and negative for the nucleocapsid (N) protein. In general, the presence of SARS-CoV-2 S antibody along with the absence of SARS-CoV-2 N antibody occurs when antibodies originate from vaccination. In contrast, the presence of both SARS-CoV-2 N and S antibodies usually implies prior infection with SARS-CoV-2. Upon discharge, persistent headaches continued, with an average NRS of 3/10 points, but the frequency of severe attacks (NRS, 7/10) decreased to once daily.
The patient was re-admitted 5 weeks after headache onset due to persistent aggravating headaches. The frequency of severe headache attacks (NRS, 7/10) increased to three times daily and interrupted the patient’s sleep. No neurologic deficit was noted. Brain magnetic resonance imaging with enhancement (T1- and T2-weighted scans) and all laboratory tests, including platelet count and coagulation profiles, showed normal findings. As headache control with rescue drugs was ineffective, the patient was prescribed topiramate (50 mg once daily) for headache prevention. For 2 months, the intensity of persistent headaches was slightly alleviated (NRS, 3/10), with once daily severe attacks (NRS, 5/10).
Four months after headache onset, the patient was admitted because of worsening headaches after contracting COVID-19. The infection was confirmed by polymerase chain reaction. Persistent headaches worsened, even after the disappearance of systemic COVID-19 symptoms. Severe attacks (NRS, 7/10) occurred up to four times daily, and persistent pain was described as 3/10 on the NRS. Psychological evaluations were performed to evaluate the presence of comorbid psychiatric disorders and indicated that the patient had moderate levels of depression and hopelessness (Beck Depression Scale score, 22 points; Beck Hopelessness Scale score, 12 points; range for moderate depression, 21 to 30). However, we concluded that these conditions were not due to primary psychological problems, but the secondary result of severe physical pain. Topiramate was changed to valproic acid (500 mg once daily) and flunarizine (5 mg once daily).
Six months after symptom onset, the patient reported a decrease in severe attacks to once daily, as well as reduced persistent headaches, and she performed her usual daily activities without missing school. Nine months after symptom onset, the frequency and intensity of headaches further decreased. Since the patient reported headaches twice a week, flunarizine was discontinued. Two months later, the patient reported no headache at all, and valproic acid was discontinued. There were no further outpatient visits for 1 month after medication discontinuation.
Here, we report the first case of an adolescent patient diagnosed with NDPH after receiving a second dose of the COVID-19 vaccine, suggesting a unique cause of NDPH. We excluded secondary causes of headaches. In addition, medication-overuse headache was also considered a possible cause, but the overuse duration did not meet the eligibility criteria. In this patient, continuous headaches lasting >3 months fulfilled the ICHD-3 criteria for NDPH. Thus, we concluded that the COVID-19 vaccine may have caused these headaches.
Long COVID headache, which manifests with an unremitting and persistent character, can be similar to NDPH [7]. However, the distinction between long COVID headache and NDPH has yet to be explored. Our case implies the possibility of a relationship between vaccination against COVID-19 and NDPH. Taken together, headaches associated with the recent COVID-19 pandemic situation may provide a good opportunity to advance headache research, including on NDPH [7].
Identifying severe and persistent headaches and considering multiple causative factors, including vaccination, are of great importance. NDPH following vaccination has rarely been reported. However, an article specifically reported human papillomavirus vaccination as a trigger for NDPH [8]. Several hypotheses for the mechanism of post-vaccination headache have been suggested: SARS-CoV-2 S protein, the consequences of cytokine reaction by an imbalance in humoral and cellular immunity, and an innate immune reaction [6]. We expect that the additional monitoring of similar cases will elucidate the incidence and prognosis of chronic and severe headaches after COVID-19 vaccination in the pediatric population.
This study was approved by the Institutional Review Board (IRB) of Chungbuk National University Hospital (IRB No. 2022-04-001). Informed written consent for the publication of this report was obtained from both the patient and the legitimate guardian.
Notes
Jon Soo Kim is an editorial board member of the journal, but he was not involved in the peer reviewer selection, evaluation, or decision process of this article. No other potential conflicts of interest relevant to this article were reported.
Author contribution
Conceptualization: HW and JKL. Data curation: JKL. Writing-original draft: HW. Writing-review & editing: JSK, WSK, and JKL.
