Early Recognition of Pediatric Strokes in the Emergency Department: Epidemiology, Clinical Presentation, and Factors Impeding Stroke Diagnosis in Children
Article information
Abstract
Purpose
Strokes are challenging to diagnose in pediatric emergency departments (EDs) as level of suspicion is low and atypical presentations are common. We analyzed clinical features, epidemiology and factors of delayed identification in arterial ischemic strokes (AIS) and hemorrhagic strokes (HS).
Methods
Single-center retrospective cohort study of children aged between 29 days and 18 years old diagnosed with stroke between July 2016 to June 2021.
Results
Among 36 children, 11 (30.5%) had AIS, 25 (69.4%) had HS. Median age for AIS was 9 years (interquartile range [IQR], 2 to 9) and HS 9 years (IQR, 1 to 11.5) (P=0.715). Focal neurological deficit was seen in 72.7% of AIS and 20% of HS (P=0.006). Only 18.2% of AIS and 52.0% of HS presented within 6 hours of symptoms. Median time from symptom onset to ED presentation was 24 hours (IQR, 12 to 28) for AIS and 7 hours (IQR, 1.8 to 48) for HS (P=0.595). Most (85.6%) arrived by own transport. Median time from presentation to neuroimaging was 7 hours (IQR, 0.9 to 7) for AIS and 4.8 (IQR, 1.3 to 16.8) hours for HS (P=0.376). Eleven patients, 9/25 (36.0%) HS and 2/11 (18.2%) AIS, did not have stroke as differential diagnosis at ED (P=0.714). Common initial diagnoses were viral illness or headaches. On univariate analysis, age <1 (odds ratio [OR], 17.5; 95% confidence interval [CI], 1.2 to 250.4; P=0.035) and absence of focal neurological deficit (OR, 13.091; 95% CI, 1.5 to 117.9; P=0.022) were significant factors for delayed identification.
Conclusion
Index of suspicion for pediatric strokes among caregivers and clinicians should be increased. Public awareness campaigns are recommended.
Introduction
Stroke is one of the top 10 causes of death in the pediatric population [1,2]. Its incidence is quoted as 2 to 13 per 100,000 persons per year [1]. Up to two-thirds of patients can suffer persistent neurological deficits [3,4] and 20% may have post-stroke epilepsy and psychological distress [5]. This imposes a significant burden on healthcare systems, with reduced quality of life and independence [5].
As with adults, strokes can be ischemic or hemorrhagic, though a larger proportion are hemorrhagic strokes (HS) in children. Common etiologies for adults are atherosclerosis or hypertension. In contrast, pediatric stroke etiologies are wider, ranging from arteriopathy, cardiac, prothrombotic disease and other systemic conditions in arterial ischemic strokes (AIS) [6], to arteriovenous malformations, hematologic disorders, and brain tumors in HS [7,8].
Recognizing acute strokes in children requires a high index of suspicion. Presentation of pediatric stroke is protean and differential diagnoses for stroke-like symptoms in children is broad. Younger children tend to present with non-specific symptoms such as seizures or altered mental state, and older children with focal neurological deficits [9].
Perhaps the greatest obstacle to optimal treatment is lack of awareness and delayed recognition. Median time from symptom onset to diagnosis of AIS ranges from 22.7 to 24.8 hours in multiple studies [10,11]. Delayed recognition occurs both with caregivers and physicians. Parents often do not recognize symptoms of pediatric stroke, resulting in delayed emergency department (ED) presentation. For physicians, it was shown in Rafay et al’s [12] retrospective study of 209 children with AIS that stroke diagnosis was suspected on initial assessment in only 79 (38%) children.
Pediatric stroke is a medical emergency and should be treated rapidly to maximize favourable outcomes [13]. Although there is paucity of data regarding morbidity and mortality because of delays in treating strokes in children, we know that this delay has ramifications on research into hyperacute stroke therapies such as thrombolysis or endovascular thrombectomy [14]. The Thrombolysis in Pediatric Stroke (TIPS) trial had to close early as most strokes were not identified within the therapeutic window, and there were greater risks than benefits of treatment [15]. The TIPS trial identified lack of stroke awareness and readiness as a problem, and was a catalyst for implementation of acute pediatric stroke protocols such as clinical pathways, order sets and round-the-clock magnetic resonance imaging (MRI) capability in various centers [9]. With these implemented, time to stroke diagnosis on MRI after arrival at ED was decreased from 17 to 4 hours [16]. However, majority of delays still occur prior to hospital presentation, making increased public awareness essential.
In this study, we aimed to evaluate epidemiology, risk factors, clinical presentations, and outcomes of pediatric strokes in a tertiary children’s hospital in Singapore. We also aimed to identify factors that confounded the diagnosis of stroke at initial ED presentation.
Materials and Methods
We performed a retrospective analysis of all patients between 29 days to 18 years old who presented to the pediatric ED of KK Women’s and Children’s Hospital, Singapore, between July 2016 to June 2021, and were subsequently confirmed to have stroke on neuroimaging. AIS is defined as presence of neurological deficit consistent with ischemia in an arterial distribution, or acute non-localizing encephalopathy (including symptomatic new-onset seizures), with confirmation of infarction on imaging or autopsy, occurring in a person between 29 days through 18 years of life [17]. HS is defined as atraumatic abrupt onset of severe headache, altered level of consciousness and/or focal neurologic deficit associated with bleeding into the brain by a ruptured blood vessel. This results in focal collection of blood within the brain on imaging not due to trauma or hemorrhagic conversion of cerebral infarction. HS includes intracerebral hemorrhage (ICH), intraventricular hemorrhage, or subarachnoid hemorrhage [7,18].
Patients were identified from SingHealth-IHiS Electronic Health Intelligence System (eHints) database using International Classification of Diseases 10th Revision (ICD-10) diagnosis codes related to AIS or HS (ICD-10 codes: arteriovenous malformation of cerebral vessels [Q28.2], cerebral infarction [I63], ICH [I61], intracranial hemorrhagic [nontraumatic; I62], subarachnoid hemorrhage [I60], stroke [not specified hemorrhage or infarction; I64], subdural hemorrhage [I62.0], other cerebrovascular diseases [I67]) [1]. To identify children who demised in ED before admission, a second search was performed for Systemized Nomenclature of Medicine (SNOMED) ED diagnoses of AIS or HS.
Exclusion criteria were traumatic brain injuries, transient ischemic attacks, perinatal strokes, metabolic infarction in a nonvascular territory (such as Mitochondrial Encephalopathy, Lactic Acidosis and Stroke-like episodes [MELAS]), hypotensive watershed injury, periventricular leukomalacia, cerebral venous sinus thrombosis or reversible hypertensive leukoencephalopathy [9].
Demographics of age, sex, ethnicity, baseline function, date and time of presentation, mode of transportation to ED, triage vitals, triage categories, Glasgow Coma Scale (GCS), symptoms, neurological examination, medications, procedures, investigations, disposition, ED diagnosis, and inpatient diagnosis were extracted from electronic medical records using SingHealth-IHiS eHints database. Past medical history, history of anticoagulation use, family history, inpatient progress, timing/type of neuroimaging, involvement of subspecialities, stroke work up, medical/surgical intervention, length of hospital stay, outcomes, and follow-ups were extracted from electronic medical records. If exact timing was not available, duration from symptom onset to ED presentation were estimated based on documentation in clinical notes rounded up to nearest hour. Patients were classified whether stroke was recognized as a diagnosis or differential diagnosis, versus not written as a possible differential.
All data were exported into a password-protected Microsoft Excel (Microsoft Corporation, Redmond, WA, USA) file and anonymized by removing patient identifiers. Statistical analyses were performed using IBM SPSS Statistics version 28.0 (IBM Corp, Armonk, NY, USA). Descriptive statistics were used for baseline characteristics and clinical presentations. Categorical variables were presented in frequencies and percentages. Continuous variables were described using mean (with standard deviation), or median (with interquartile range [IQR]), depending on normality. Categorical variables were analyzed using Fisher’s exact test and continuous variables using Student’s t-test or Wilcoxon rank sum, depending on normality. Univariate regression analyses were performed to identify factors associated with diagnosis after admission. Variables with P<0.1 in univariate analysis were included in a multivariate logistic regression model to identify independent predictors. Statistical significance was taken at P<0.05. All point estimates were presented with corresponding 95% confidence intervals (CIs).
This study and waiver of informed consent were approved by SingHealth Centralised Institutional Review Board (Reference 2021/2721).
Results
1. Demographics
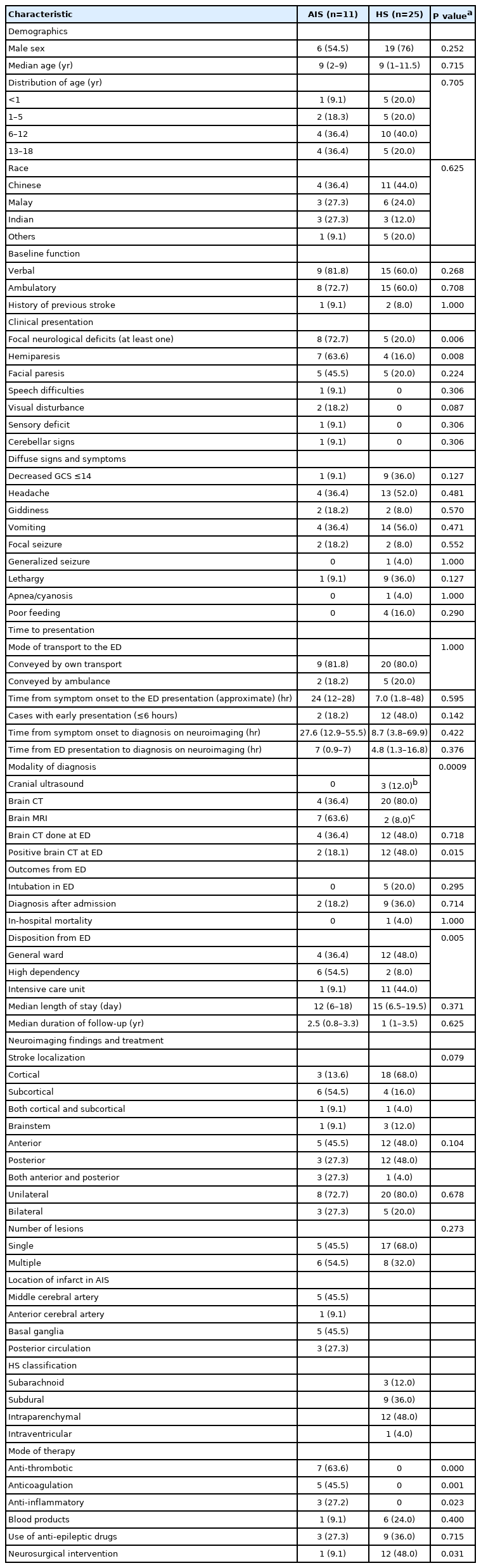
Thirty-six children were identified, 11 with (30.5%) AIS and 25 with (69.4%) HS (Table 1). Majority were male (25/36, 69.4%). Median age was 9 years for both AIS (IQR, 2 to 9) and HS (IQR, 1 to 11.5) (P=0.715). Number of infants <1 year old amongst HS cohort was five (20.0%) and one (9.1%) in AIS cohort (P=0.705).
2. Clinical presentation
Patients with AIS were more likely to have detectable focal neurological deficits at presentation (8/11 [72.7%] vs. 5/25 [20.0%] for HS, P=0.006). Hemiparesis was four times higher in AIS (63.6%) compared to HS (16.0%) (P=0.008) and facial paresis was seen in 5/11 (45.5%) of AIS compared to 5/25 (20.0%) in HS (P=0.224). Patients with AIS presented less frequently with non-specific signs and symptoms such as headache, vomiting and lethargy, compared to HS (Table 1). Fewer AIS patients were admitted to the intensive care unit (1/11 [9.1%] vs. 11/25 [44.0%] HS, P=0.005). No AIS patients required intubation, while 5/25 (20.0%) of HS patients were intubated in ED (four for GCS <8, one for respiratory distress) (P=0.295). No patients demised in ED. One HS patient demised as an inpatient.
3. Time to presentation
Median time from symptom onset to ED presentation was 24.0 hours (IQR, 12 to 28) for AIS and 7.0 hours (IQR, 1.8 to 48) for HS (P=0.595). Only 2/11 (18.2%) of AIS and 12/25 (48.0%) of HS patients presented within 6 hours (P=0.142). Majority of patients were conveyed to hospital via own transport rather than ambulance: 9/11 (81.8%) AIS and 20/25 (80.0%) HS (P=1.000).
Median time from ED presentation to neuroimaging diagnosis was 5.8hours (IQR, 1.2 to 14.2) overall, 7.0 hours (IQR, 0.9 to 7) for AIS and 4.8 hours (IQR, 1.3 to 16.8) for HS (P=0.376).
Median time from ED presentation to neuroimaging diagnosis was 8.0 hours (IQR, 1.3 to 8) for patients with known cardiac disease (n=3; P=0.857), 7.5 hours (IQR, 6.0 to 7.5) for patients with previous history of stroke (n=3; P=0.735), 6.0 hours (IQR, 1.5 to 6.0) for known brain tumors (n=2; P=0.735), and 18.5 hours (IQR, 13.5 to 36.2) for patients with known hematological disorders (n=6; P=0.546).
Four AIS patients (36.4%) were identified on computed tomography (CT) brain and seven AIS patients (63.6%) were identified on MRI brain. Two of four AIS patients had negative CT brain findings at ED for stroke but were subsequently diagnosed with stroke on MRI brain (Table 1). One patient developed acute worsening neurological symptoms inpatient and MRI brain was performed 7 hours after the initial CT brain. The other patient’s provisional CT brain report was normal but given high clinical suspicion, MRI brain was arranged 3 hours after initial CT. Conversely, majority of HS were identified on CT brain 20/25 (80.0%) (P=0.0009). Of the remaining HS patients, 3/25 (12.0%) were diagnosed by ultrasound cranium (of which one was performed as point-of-care in ED) and 2/25 (8.0%) on MRI brain, which were ordered by inpatient team as they were not admitted with provisional diagnoses of HS. These two cases did not have prior CT brains. One of them had MRI brain done due to persistent headache while the other patient had worsening lethargy and intermittent drowsiness.
4. Stroke localization
For AIS, majority were subcortical 6/11 (54.5%) and unilateral 8/11 (72.7%); 5/11 (45.5%) had single infarcts and 6/11 (54.5%) had multiple infarcts. For HS, 3/25 (12.0%) had subarachnoid hemorrhage, 9/25 (36.0%) had subdural hemorrhage, 12/25 (48.0%) had intraparenchymal hemorrhages, and 1/25 (4.0%) had intraventricular hemorrhage.
5. Inpatient treatment
Children with AIS received anti-thrombotic (7/11, 63.6%) and anticoagulation (5/11, 45.5%) therapy. Three (3/11, 27.3%) children with AIS secondary to central nervous system (CNS) vasculitis received anti-inflammatory medications: two pulsed intravenous methylprednisolone and one oral prednisolone during the same admission. Blood transfusion was required for 6/25 (24.0%) of HS and 1/11 (9.1%) of AIS patients (P=0.400). Nearly half of HS required acute neurosurgery for shunt or decompression (12/25, 48.0%) compared to one for AIS (P=0.031).
6. Etiology
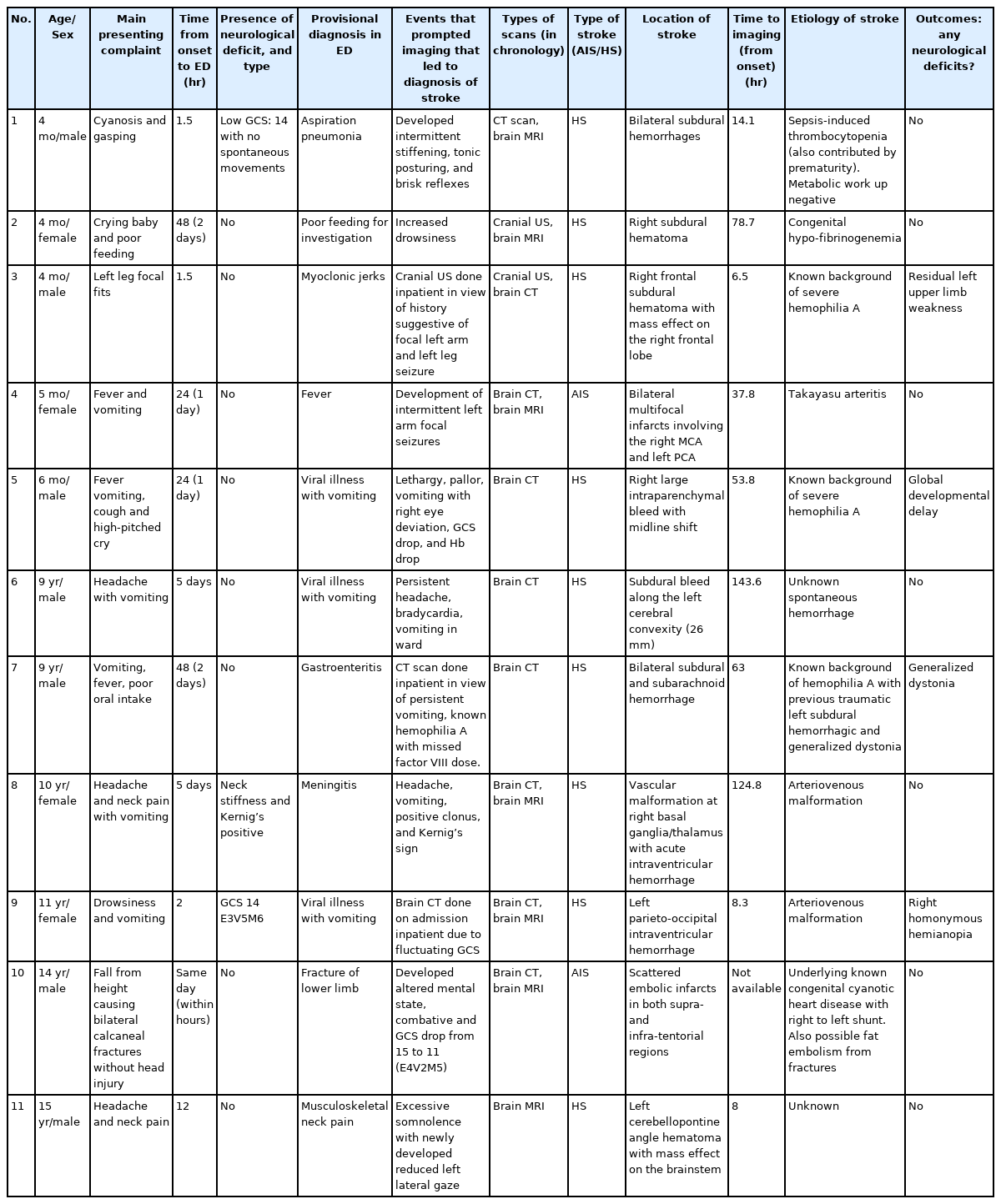
Etiologies of AIS and HS were shown in Table 2. For AIS, 4/11 (36.4%) were secondary to newly diagnosed arteriopathy or vasculitis. Two (18.2%) had underlying cardiac conditions. One (9.1%) had a known underlying prothrombotic protein C deficiency with an infective trigger. Four (36.4%) had unknown etiologies. For HS, majority (13/25, 52.0%) were due to newly diagnosed abnormal vascular malformation. Seven (28.0%) were due to coagulopathies or hematological disorders, two of which newly diagnosed. Two (7.7%) were due to brain tumor; one newly diagnosed. Three (12.0%) had unknown etiologies.
7. Neurological sequelae
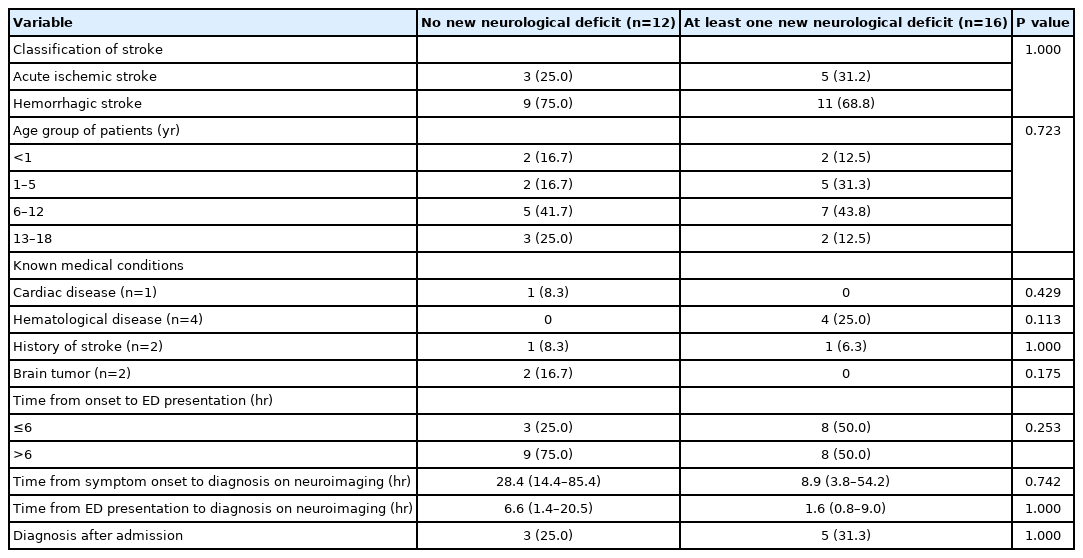
Among 28 patients with at least 1 year follow-up (Table 3), more than half had at least one residual neurological deficit: 5/8 (62.5%) for AIS and 11/20 (55.0%) for HS. Children with AIS had predominantly motor deficits (5/8, 62.5%) while HS patients suffered limitations including speech difficulties, epilepsy and cognitive and behavioral impairment. We analyzed factors of residual neurological deficits after 1 year (Table 4). Classification of stroke, age group, time of symptom onset to ED presentation and whether patients were diagnosed in ED or inpatient, were not significantly associated with residual neurological deficits. Patients with known hematological disease were more likely to have residual deficits (4/4, 100%) (P=0.113). Patients with residual neurological deficits had lower time of symptom onset and time of ED presentation to diagnosis on neuroimaging.
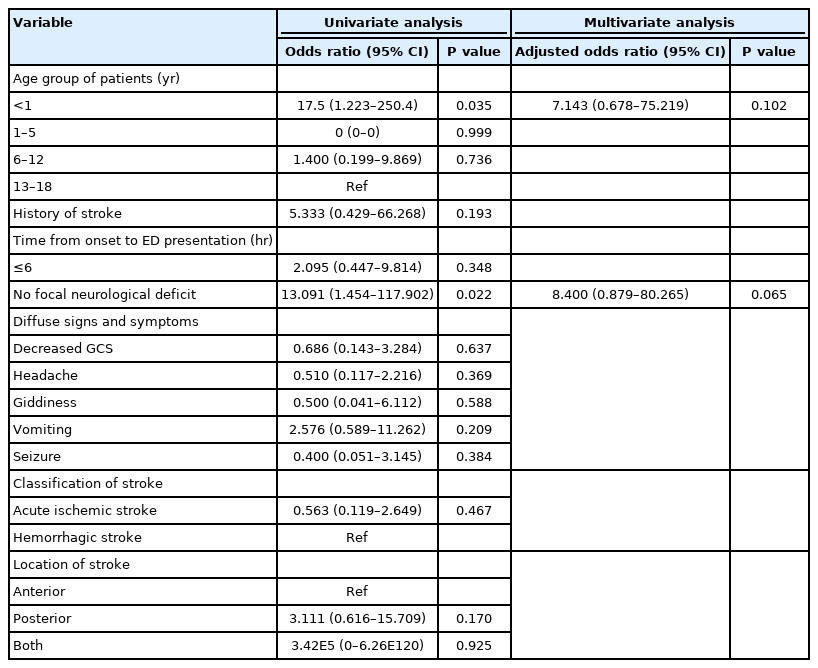
8. Factors of stroke not recognized as possible differential diagnosis in ED
Eleven patients did not have stroke recognized as a possible differential in ED. There were five (45%) children <6 months old, six (55%) children >9 years old, nine (81.8%) with HS, and two (18.2%) with AIS (P=0.714) (Table 5). We analyzed factors of diagnosis after admission in Table 6. Age <1 year (odds ratio [OR], 17.5; 95% CI, 1.2 to 250.4; P=0.035) and absence of focal neurological deficit (OR, 13.091; 95% CI, 1.5 to 117.9; P=0.022) were significant factors on univariate but not multivariate analysis. Generally, younger infants presented with symptoms such as poor feeding, crying, vomiting, and aspiration symptoms. They were mostly initially diagnosed as respiratory tract infections or viral illnesses. Older children presented with symptoms such as headache, neck pain or vomiting, and were commonly diagnosed as secondary headaches due to viral illnesses or musculoskeletal pain. Most did not display neurological deficits except two with slightly reduced GCS scores of 14.
Discussion
We characterized presentations of pediatric stroke and identified key factors which impede diagnosis of stroke in this age range. Notably, age <1 year and absence of focal neurological deficit impeded diagnosis of stroke in ED. Presenting features varied according to stroke type; focal features were more common in AIS, as in other studies [11,19]. Our data showed that 36.1% presented with focal features and 30.5% with hemiparesis, lower than Mallick et al’s [11] study, in which 85% presented with focal features and 72% with hemiparesis. Our data also reflected that pediatric strokes are often non-specific—common presentations were lethargy (27.8%) and altered level of consciousness (27.8%). The previous local study in 2009 found lethargy in 42.3% and altered level of consciousness in 38.5% [20]. Children <6 years old with AIS can also present with seizures [21]. Seizures in our study was 5/36 (13.9%), compared to 57.7%, which was the most common presenting feature in the previous local study [20]. Half of our HS patients presented with headache and vomiting. In a systematic review, headache was found to be the most frequent complaint in 46% to 80% of children with nontraumatic ICH [18].
Pre-hospital delay from time of symptom onset to ED presentation is the largest barrier to pediatric stroke care here. It is important for early stroke interventions. such as neuroprotective measures to maintain cerebral perfusion, normoglycemia, or expedient early surgical decompression in HS [9]. Our median time of symptom onset to ED presentation is 24 hours for AIS and 7 hours for HS, suggesting delayed caregiver recognition. Furthermore, less than 20% were transported via ambulance, suggesting it was not identified as emergency by most parents. Our data was similar to international studies that also cited 22.7 to 24.8 hours as median time of symptom onset to diagnosis in AIS [10,11]. Deng et al. [19] additionally found that symptom onset to ED was significantly prolonged: only 3.7% of AIS and 14.4% of HS patients presented within 24 hours. More public health awareness in increasing parent/caregiver knowledge about childhood stroke would be useful.
Pediatric ED physicians play a critical role in early diagnosis. Studies of pediatric thrombolytic therapy suggested that risks outweigh benefits [15]. Hence focus should be on early recognition, so patients with AIS can receive timely medical treatment, regardless of MRI confirmation. Hori et al. [22] found that only 27% of AIS were diagnosed within 6 hours after symptom onset, and attributed this delay to absence of clinical suspicion. Around one-third of our patients did not have stroke as a clear differential diagnosis, largely due to non-specific symptoms and absence of focal neurological deficits. A higher proportion were HS (36.0% HS vs. 18.2% AIS) and nearly half were infants. HS patients can have decreased GCS, non-specific symptoms of headache, vomiting, and even neck pain. Interestingly, two patients (age 10 and 15) with HS presented with headache and neck pain. A postulated pathophysiology is that blood tracking down spinal column causes neck pain and stiffness from meningeal irritation.
AIS patients tend to present with focal neurological deficits (P=0.006), which raised suspicion of stroke. Nonetheless, Mackay et al. [23] reported in a prospective cohort study of 287 children presenting to ED with focal neurological deficits that sensitivity of stroke diagnosis was only 62% with a specificity of 98%. Common mimics included migraine, seizures, Bell’s palsy, conversion disorder and syncope. Acute neurological diagnoses (HS/AIS) should be considered as a possible diagnosis in ill-looking children, especially infants, presenting with non-specific symptoms.
Median time from ED presentation to neuroimaging diagnosis was 5.8 hours (IQR, 1.2 to 14.2) overall, and presence of known cardiac disease, stroke, or brain tumor did not lead to earlier diagnosis. However, median time from ED presentation to neuroimaging diagnosis was 18.5 hours (IQR, 13.5 to 36.2) for patients with known hematological disorders (n=6), and none had neuroimaging from ED. Neuroimaging was performed due to evolving symptoms or persistent non-specific symptoms inpatient. Four of the five of patients with hypofibrinogenemia or hemophilia had subdural hemorrhage. We postulate that patients with bleeding disorders may present with slow bleed, compared to patients with ruptured arteriovenous malformation that tend to present more acutely.
Previous literature had cited normal head CT scan as a risk factor for delayed diagnosis in AIS [24]. Most ischemic strokes presented with at least one neurological deficit with ipsilateral signs (Table 1). In such cases, MRI brain is the preferred modality of imaging [24]. However, patients present to ED undifferentiated. CT brain is still a valuable modality in urgent neuroimaging in our context given high proportion of HS, and remains first line for cases with suspected stroke without focal neurological deficits. In Mallick et al.’s [11] cohort study of 96 children with stroke, CT is diagnostic in 95% of HS. Majority of our HS patients were diagnosed via point-of-care cranial ultrasound (with no radiation risk) and CT, suggesting that HS was astutely suspected by attending physicians. Our study showed that the majority of HS present early, hence early presentation may be another indicator to perform CT brain. Another proposed indication is for known hemophiliacs who were ill-appearing patients or vomiting without clear gastroenteritis symptoms, in which cranial ultrasound or CT should be considered early for suspected HS.
Nevertheless, appropriate treatment should still be commenced. In our cohort, two AIS patients had negative CT scans performed at ED. CT brain was performed for 2 hours acute onset of left sided weakness, and for seizure with right hemiplegia lasting 1 hour. They were eventually diagnosed with AIS due to CNS vasculitis and cardioembolism respectively. Appropriate treatment of intravenous hydration and neuroprotective measures was still started regardless of MRI scan timing and findings. After MRI, further treatment with enoxaparin for CNS vasculitis and heparin for cardioembolism was commenced. Hence, median time of symptom onset to ED presentation still remains a larger barrier to care than time to neuroimaging.
Our 5-year retrospective study of 36 patients with AIS and HS had similar incidence to another Singapore study of 26 patients between 1999 and 2006 [20]. Male sex predominance was also reported in International Pediatric Stroke Study (IPSS) [25]. Normann et al. [26] suggested that boys have higher risk of AIS due to elevated circulating androgen levels, associated with 4- to 5-fold increased risk of cerebrovascular disease after adjustment for pubertal status, cholesterol, and hematocrit levels. In HS, risk factors such as hemophilia also carry X-linked genetic predisposition.
The most common causes of AIS in our study were arteriopathy (36.4%) and unknown (36.4%), followed by cardiac disease (18.2%). Arteriopathy and cardiac disease were the top identified risk factor categories in IPSS at 53% and 31% respectively [6]. The study also found that risk varied by age; arteriopathy was most common for age 5 to 9, cardiac disease and infections were more common in younger children, and chronic head and neck disorders were more common in older children. Large proportion of AIS were idiopathic, ranging 24% to 41% [27,28]. For HS, intracranial vascular malformation (52%) was most common, similar to literature (40% to 90%) [18,20,29].
In terms of outcomes, both AIS and HS patients can have morbidity and functional impairment. Literature found that prolonged delays >24 hours from ICH symptom onset to presentation was associated with poorer functional outcomes [30]. However our data shows that age group, time of symptom onset to ED presentation/diagnosis and whether patients were diagnosed in ED or inpatient, were not significantly associated with residual neurological deficits. Patients with residual neurological deficits had lower time of symptom onset and time of ED presentation to diagnosis on neuroimaging, likely because of more extensive strokes at presentation. We evaluated outcome based on presence of neurological deficit, but opted not to analyze severity and whether patients had decreased independence of activities of daily living due to large age ranges. Hence, we do recognize that presence of neurological deficit does not necessarily infer reduced independence and quality of life.
Our study had several limitations. As a retrospective study, there are inherent limitations in information available in medical records. Fifteen patients had dates but not exact time documented hence duration of symptoms were rounded up to the nearest hour. Similarly, presence of residual neurological deficits were inferred from latest follow-up notes. As scoring methods was inconsistent the data were not analyzed in this study. We recommend outcome measurement for pediatric stroke registries. Functional Independence Measure (WeeFIM) and Pediatric Glasgow Outcome Scale Extended [31,32], which have both been utilized and published for childhood encephalitis at our institution, are potentially preferred tools for functional outcome assessment.
The merits of our paper included identification of potential factors for delayed physician recognition of stroke. Our paper is unique to previous studies as we focused on the presentation and ED level of care in order to address known challenges of early diagnosis. We obtained detailed information on presentation, etiology and clinical course of these 36 patients. We analyzed the thought process of ED physicians in terms of provisional diagnosis, to identify additional red flags that should prompt early neuroimaging. We identified that age <1 year and absence of focal neurological deficit were potential risk factors for delays in stroke identification in the ED on univariable analysis. These values were clinically relevant and would likely have approached statistical significance on multivariable analysis (P=0.065) with larger sample size, thus was still valuable in guiding assessment of children with potential stroke. Our data supports existing literature that CT is the first line for urgent neuroimaging in suspected HS, even without focal neurological deficits. Threshold for neuroimaging should be lower for ill-appearing patients with known bleeding disorders. We postulate that lack of parental awareness and recognition of symptoms as an emergency are potentially the largest barriers to timely pediatric stroke care. Singapore is a small island state with efficient transport system and well-developed pre-hospital care, hence transportation time is not a limitation. Awareness should be focused on delayed recognition and pre-hospital delays.
In conclusion, our first key message is that pre-hospital delay from time of symptom onset to ED presentation is the largest barrier to stroke care here, rather than time to neuroimaging. Hence, focus should be on early recognition, so patients can receive timely medical treatment regardless of MRI confirmation. Secondly, age <1 year and absence of focal neurological deficit impeded diagnosis of stroke in ED, hence index of suspicion should be high for ill-appearing infants in this age group. Methods to improve early recognition include increasing public health awareness for caregivers, and for ED physicians to be cognizant about diverse etiologies, differential diagnoses, and varied presentations of childhood stroke.
Notes
Derrick Wei Shih Chan is an editorial board member of the journal, but he was not involved in the peer reviewer selection, evaluation, or decision process of this article. No other potential conflicts of interest relevant to this article were reported.
Author contribution
Conceptualization: SQT, WQC, SLC, ASYA, SG, DWSC, and RMRT. Data curation: SQT and WQC. Formal analysis: SQT. Methodology: SQT, WQC, SLC, ASYA, SG, DWSC, and RMRT. Project administration: SQT. Visualization: SQT and WQC. Writing-original draft: SQT and WQC. Writing-review & editing: SQT, WQC, SLC, ASYA, DWSC, and RMRT.
Acknowledgements
We would like to thank KK Women’s and Children’s Hospital Department of Emergency Medicine and Pediatric Neurology for their support.