Metopic Craniosynostosis and Hydrocephalus in a Premature Opioid Dependent Baby
Article information
Craniosynostosis involves premature closure of cranial suture lines, causing increased intracranial pressure and hydrocephalus. This results in the skull or facial bones changing from a normal appearance to a more triangular forehead, termed as trigonocephaly (Fig. 1). A newborn male was delivered prematurely at 35 weeks and 3 days gestational age, weighing 2.3 kg at birth.
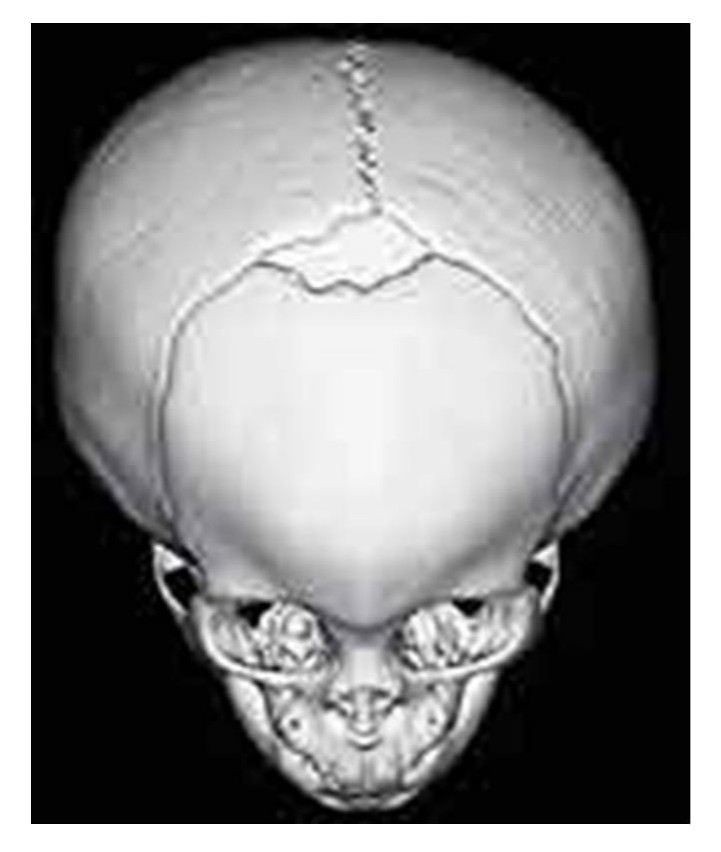
This computed tomography scan with three-dimensional reconstruction demonstrates trigonocephaly with fused metopic sutures.
The cranial contour showed evidence of trigonocephaly [1]. Magnetic resonance imaging (MRI) findings portrayed complete fusion of the metopic sutures, mid-sagittal sutures, lambdoidal sutures and partial fusion of the coronal sutures. Clinically, a fusion of the calvaria along the auriculo-auricular suture is referred to as the coronal suture fusion. Conversely, a metopic suture fusion presents with a triangular forehead, a palpable midline ridge, hypotelorism-induced ethmoidal hypoplasia and minimal anterior cranial fossa [2]. Diagnosis of craniosynostosis is based on typical facial and cranial morphology and can be done through Caldwell-Luc antrostomy as well. Early calcification of developing sutures occurs with oxidative stress due to postnatal ventilation in premature births. Altered calcification leads to trigonocephaly with metopic suture fusion, which is treated with metopic craniosynostosis surgical repair: Caldwell-Luc antrostomy was performed as a diagnostic and therapeutic approach [3]. This repair confirmed and treated the metopic craniosynostosis; however, the surgery was complicated by post-operative hydrocephalus in this patient at age 2 years. Although currently inaccessible, the brain MRI was indicative of hydrocephalus. Evidence of high intra-cranial pressure such as papilledema secondary to optic disc swelling and left abducens nerve palsy appeared secondary to intracranial pressure. Due to the severity of this post-operative hydrocephalus, an external ventricular drain and a ventriculoperitoneal shunt were urgently placed in this patient to reduce intracranial pressure. Maternal use of opioids is shown to have an association with opioid use in the National Birth Defects Prevention Study from 1997 to 2005, a case control study of 17,449 case mothers showed statistical significance of conoventricular septal defects, hypoplastic left heart syndrome and spina bifida. This study showed statistically significant ratios associating congenital malformations with maternal opioid treatment one month before pregnancy and during the first trimester [4]. Pre-natal nutritional status was within normal limits and the pre-delivery medications consisted of only Tylenol (Johnson & Johnson, Brunswick, NJ, USA) as needed. The atypical nature of post-operative hydrocephalus in this patient warranted an examination of possible syndromic craniosynostosis; however, syndromic craniosynostosis was ruled out through single nucleotide polymorphism genotyping analysis and whole genome sequencing. Other differentials were ruled out by routine newborn screening and verification of epicanthal folds, a normal cephalic index despite biparietal broadening, the surprised coon sign and concurrent bitemporal shortening. This suggests that maternal opioid dependence may be associated with other congenital malformations such as the metopic craniosynostosis seen in this case [5]. A year later the patient presented with macro-encephaly. The patient also needed occlusive therapy to correct his severe strabismus. The patient was obese at >97th percentile with a tendency to gain weight easily, and also short in stature. Weight control strategies were implemented.
Neuropsychological signs of craniosynostosis include affected development of behavior, speech and language; deficiencies in cognition; neurodevelopmental delays such as attention deficit hyperactivity disorder, oppositional defiant disorder, autism spectrum disorder, and conduct disorder [5]. Some of these signs were seen in this patient. The patient experienced extensive speech delay as well: at 2 years old he was able to say only two words.
After revision surgery of the trigonocephaly, despite management of the complication of post-operative hydrocephalus, this patient with non-syndromic craniosynostosis had persistent, related conditions including obesity, speech delay and a need for occlusive therapy.
The patient was informed and agreed to voluntary disclosure for the purpose of research publication and the betterment of healthcare.
Notes
No potential conflict of interest relevant to this article was reported.
Author contribution
Conceptualization: TP. Data curation: TP and SSM. Formal analysis: TP and SSM. Funding acquisition: SM and PM. Methodology: TP and SSM. Project administration: SM and PM. Visualization: TP, SSM, SM, and PM. Writing-original draft: TP and SSM. Writing-review & editing: TP and SSM.
