 |
 |
- Search
| Ann Child Neurol > Volume 28(4); 2020 > Article |
|
Cerebral sinovenous thrombosis (CSVT) is an uncommon disease (0.4 to 0.7 cases per 100,000 live births) characterized by blood clotting in the cerebral venous sinuses [1]. The diagnosis is often delayed owing to its nonspecific symptoms. However, fatal neurological sequelae, including developmental delays, visual impairment, and cerebral palsy, may develop [1]. Diabetes mellitus (DM) can be responsible for this hypercoagulable state [1]. A certain gene involved in the insulin synthesis and secretion pathway might be involved in some cases and can contribute to CSVT treatment. Particularly, neonatal DM (NDM) is a rarer disease, which is encountered with hyperglycemia within the first 6 months of life [2]. Herein, we report the case of a male infant diagnosed with CSVT caused by NDM. He was treated promptly owing to early detection, without finding a causative gene yet.
A 50-day-old boy visited our emergency center with an abruptly sunken anterior fontanelle. He was a first-born child and had no specific underlying diseases and family DM history, despite his small size considering the gestational age at birth (37 weeks, 2,040 g). His weight, height, and head circumference were within 3 percentiles. Although his initial vital signs were stable, he seemed severely dehydrated with dry lips and mottled skin. His mental state was alert and neurological examination was unremarkable. Eye tracing and social smile were possible, indicating normal development.
The initial laboratory analysis revealed severe hyperglycemia (1,352 mg/dL) and hypernatremia (160 mEq/L). Blood gas analysis revealed metabolic acidosis (pH, 7.2; bicarbonate concentration, 17.5 mmol/L), and urinalysis revealed glycosuria without ketonuria. Serum ketone tracing led to the suspicion of diabetes. The possibility of metabolic diseases was eliminated using negative tandem mass spectrometry. Hemoglobin A1c (HbA1c) and fasting C-peptide levels were 5.8% and 0.7 ng/mL, respectively. Antibody tests for islet cells and insulin, and anti-glutamic acid decarboxylase were negative. He was treated with normal saline (10 cc/kg) infusion for the first hour, followed by continuous intravenous infusion of regular insulin (0.05 U/kg/hr) with half-normal saline according to the principle of diabetic ketoacidosis treatment.
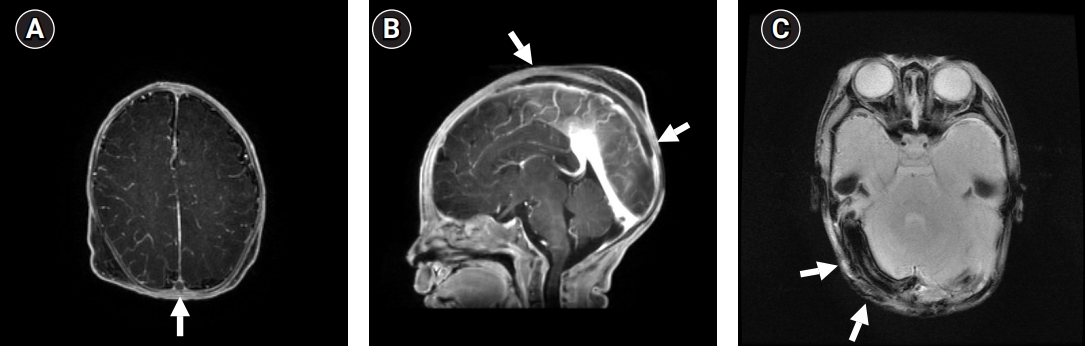
Meanwhile, he suddenly developed seizure-like trembling movements in both legs. This generalized tonic-clonic seizure disappeared after 3 days; however, repetitive saw-tooth-like electrical seizure activities with sudden lower and upper margin elevation were recorded for 7 days on the amplitude-integrated electroencephalograph (aEEG) followed by a marked depression on aEEG tracing (Fig. 1), corresponding to non-convulsive electrical status epilepticus. Diffusion brain magnetic resonance imaging (MRI) was performed immediately, and lesions suspicious of venous thrombosis were observed. Subsequent contrast-enhanced MRI revealed extensive CSVT (Fig. 2).
Continuous intravenous heparin and anticonvulsant treatments were administered promptly. The heparin loading dose (75 U/kg over 10 minutes) was followed by a maintenance dose for 4 weeks, determined by the activated partial thromboplastin time (aPTT) according to the Protocol for Systemic Heparin Administration and Adjustment in Children [3]. Intravenous phenobarbital was started and lorazepam was intermittently administered when a convulsive movement presented. As this was not well-controlled, topiramate and levetriacetam were added. The electroclinical seizures disappeared and lesions improved on follow-up MRI at 4 weeks. Finally, he was discharged after switching to subcutaneous injection of 1 mg/kg low-molecular weight heparin twice a day. The insertion of an insulin pump ensured good blood sugar control. Despite receiving regular basic rehabilitation, the patient demonstrated delayed milestones, i.e., those of a 7-month-old when he was 28-month-old, for all the developmental areas (gross motor, fine motor, cognition, language, sociality, and self-care) on the Korean Developmental Screening Test for Infants and Children. He still requires 0.5 to 0.6 U/kg of insulin per day for normoglycemia maintenance. All known genetic tests related to NDM, such as ABCC8, KCNJ11, 6q24 methylation, and targeted exome sequencing, were negative.
Among CSVT treatments, use of anticoagulation therapy in children is still controversial and limited. However, several studies have reported better outcomes and safety with careful aPTT monitoring [3]. Determining the etiology of various underlying conditions causing CSVT in children is also crucial for the treatment. Dehydration is found in a sizable proportion of neonates and can induce sinovenous occlusion by altering systemic circulation [1]. Considerable elevation of random blood sugar levels alone led to the NDM diagnosis in this case. Importantly, when NDM is accompanied by severe dehydration despite the absence of certain neurological symptoms, neuroimaging and cerebral function monitoring should be conducted promptly. Treatment strategies including thrombolysis should be established and at least be considered even in newborns [1].
NDM can be classified into transient (45%), permanent (45%), and syndromic forms (10%). Our patient can be considered to have permanent NDM, as the blood sugar level elevation lasted for more than 6 months. Further HbA1c elevation to 6.5% over 6 months suggests that type 1 DM had occurred at a very early age.
This report has some limitations. First, genetic analyses of the patientŌĆÖs parents were not conducted. Second, the extent of whole exome sequencing was not sufficient to detect a potential mutation.
There are three reports on CSVT resulting from hyperglycemia [2,4,5]. Anik et al. [2] described the case of a 2-month-old patient who presented with focal clonic seizures, which was the most similar to ours. Conversely, Sasiadek et al. [4] and Keane et al. [5] described the cases of patients aged >5 years, who lost consciousness a few hours after visiting the hospital. Neuroimaging examinations, such as computed tomography or MRI, were necessary for diagnosis and performed immediately after the appearance of each symptom; CSVT was confirmed in all cases.
Subcutaneous enoxaparin [2] and heparin [4,5] were used to dissolve cerebral thrombosis. Treatment was switched to sulfonylurea administration in one study [2] because the genetic analysis revealed a de novo ABCC8 (modulator of the potassium channel) mutation. Most patients with channelopathy responded well to sulfonylurea treatment. Several known genes linked to NDM development were analyzed in our patient, without any satisfactory results.
In conclusion, prompt neurological evaluation including neuroimaging studies and cerebral function monitoring should be performed for appropriate NDM management with severe dehydration, before the manifestation of neurological symptoms. Molecular gene analysis for rare diseases may assist in determining targeted-treatment strategies.
This case report was approved by the Institutional Review Board of Bundang CHA Medical Center (CHA 2018-06-008) after agreement with the infantŌĆÖs parents.
Notes
Author contribution
Conceptualization: SR, EGY, KYC, and MKJ. Data curation: CY, SR, EGY, and MKJ. Formal analysis: SR and MKJ. Funding acquisition: KYC. Methodology: KYC and MKJ. Project administration: SR, EGY, KYC, and MKJ. Visualization: CY, SR, HJC, KYC, and MKJ. Writing-original draft: CY. Writing-review & editing: CY, HJC, KYC, and MKJ.
Acknowledgments
This work was supported by the Institute for Information & Communications Technology Promotion (IITP) grant funded by the Korean government (2018-2-00861, Intelligent SW Technology Development for Medical Data Analysis).
We would like to thank Editage (www.editage.co.kr) for English language editing.
Fig.┬Ā1.
Amplitude-integrated electroencephalography (aEEG) of the patient. Several repetitive saw-tooth-like electrical seizure activities (triangles) were detected on the aEEG (A) and its corresponding raw electroencephalography (EEG) channel (B) without clinical seizures.
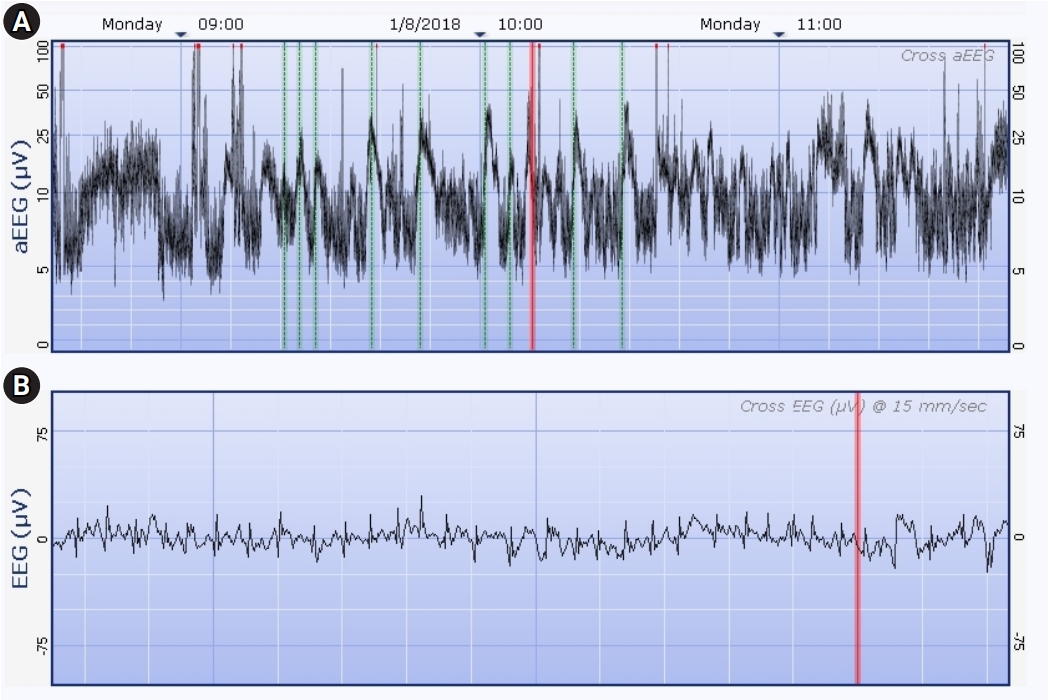
Fig.┬Ā2.
Brain magnetic resonance imaging (MRI) of the patient. Extensive filling defects can be seen along the superior sagittal sinus on the contrast enhanced T1-weighted axial image (arrow in A) and on sagittal image (arrows in B). T2* gradient-echo sequence imaging (arrows in C) demonstrated significant blooming in the transverse sigmoid sinuses. Follow-up magnetic resonance imaging conducted after 1 month shows considerable improvement and chronic changes (atrophic sinuses) in the presumed venous thrombosis (not shown).
References
1. Saadatnia M, Fatehi F, Basiri K, Mousavi SA, Mehr GK. Cerebral venous sinus thrombosis risk factors. Int J Stroke 2009;4:111-23.


2. Anik A, Catli G, Abaci A, Yis U, Oren H, Guleryuz H, et al. A novel activating ABCC8 mutation underlying neonatal diabetes mellitus in an infant presenting with cerebral sinovenous thrombosis. J Pediatr Endocrinol Metab 2014;27:533-7.



3. Roach ES, Golomb MR, Adams R, Biller J, Daniels S, Deveber G, et al. Management of stroke in infants and children: a scientific statement from a Special Writing Group of the American Heart Association Stroke Council and the Council on Cardiovascular Disease in the Young. Stroke 2008;39:2644-91.


- TOOLS







