Paroxysmal Seizure-Like Activities Caused by Unrecognized Acute Myocarditis Masquerading as Febrile Seizures in Children
Article information
Abstract
Purpose
Recognition of cardiogenic syncope caused by acute myocarditis masquerading as febrile seizures (FS) in children can be difficult in the emergency department (ED) before a cardiac work-up. We aimed to identify clinical and laboratory characteristics of children with seizure-like activity and fever caused by myocarditis that would enable their condition to be distinguished from benign FS.
Methods
We identified seven children who visited the ED for paroxysmal seizure-like activity with fever and were diagnosed with acute myocarditis between 2012 and 2015, as well as 204 children who were diagnosed with benign FS during the same period. A detailed retrospective review of the medical charts of both groups was conducted.
Results
Age at onset of seizure-like activity was much higher in the myocarditis group than in the FS group (4.4±1.9 years vs. 2.4±1.1 years, P=0.033). Body temperature at seizure-like activity onset was significantly lower in the myocarditis group than in the FS group (37.9°C±0.2°C vs. 38.7°C±0.6°C, P<0.001). Prodromal symptoms were significantly different, with nausea/vomiting (85.7% vs. 1.5%, P<0.001), abdominal pain (42.9% vs. 0.0%, P=0.021), and lethargic mentality (57.10% vs. 0.0%, P=0.015) being more frequent in the myocarditis group. The initial laboratory findings significantly differed between the two groups, with higher levels of liver enzymes, lactate dehydrogenase, creatinine, uric acid, creatine kinase, and potassium in the myocarditis group.
Conclusion
Prodromal symptoms and initial laboratory results were significantly different between the myocarditis and FS groups. A good clinical history and laboratory findings can be helpful for differentiating cardiogenic syncope from benign FS.
Introduction
Among the pediatric population, acute myocarditis is an uncommon but fatal disease. The actual incidence of myocarditis is unknown but is probably underestimated. Most estimates are based on autopsy studies and range from 0.1% to 5.6% in children and adults [1-3]. Some studies have shown peaks in very young children and adolescents [2,4]. In the Emergency Department (ED), early diagnosis of myocarditis in children might benefit from the early administration of intravenous immunoglobulin and inotropic agents, and intervention of mechanical circulatory support [5]. However, diagnosis is difficult because clinical presentation is nonspecific and inconsistent, and misdiagnosis may lead to legal dispute [6].
The most common clinical findings in a case series included tachypnea, intercostal retractions, tachycardia, and grunting, and those symptoms led to 71% of children being misdiagnosed as having either sepsis or pneumonia/asthma [7]. Alternatively, children can present with nausea and vomiting and may be mistakenly diagnosed as having gastroenteritis [8]. Some of these patients may experience unconsciousness with involuntary or seizure-like activities (convulsive syncope) due to generalized cerebral hypoxia of cardiac etiology, which can appear similar to epileptic seizure, leading to a misdiagnosis of epilepsy. In particular, when a young infant or preschool child visits ED presenting with seizure-like activity such as loss of consciousness (LOC) and mild to high fever caused by myocarditis, it may look similar to the symptoms of benign febrile seizure (FS) in children, and a pediatric neurologist should be notified. Unless we consider the possibility of cardiogenic causes, the evaluation and appropriate management of cardiac etiology may be further delayed.
We experienced seven children with acute myocarditis presenting with seizure-like activity and mild to high fever, which was initially considered as possible FS, who were evaluated at the pediatric neurology department before cardiac examination. To the best of our knowledge, there has been no study of the differences in clinical and laboratory findings between children with acute myocarditis with seizure-like activities and FS until now. This study aimed to identify the initial clinical and laboratory characteristics of children with seizure-like activity and fever caused by acute myocarditis that could be differentiated from those of benign FS, except by regular cardiac work-ups such as electrocardiogram (ECG) and echocardiogram.
Materials and Methods
We retrospectively reviewed the medical charts of children who were diagnosed with acute myocarditis and presented a seizure-like activity with mild to high fever as the main complaint, between 2012 and 2015 in a single tertiary care hospital. In considering of the complex FS, we included not only generalized onset seizure but also focal onset seizure such as LOC/impaired awareness. In order to evaluate the children who could suspect the possible FS as well as typical FS, the range of body temperature was more than or 37.7°C. Of 24 children with myocarditis, seven patients (29.2%) visited our ED presenting with seizure-like activity as the main initial symptom. Myocarditis was diagnosed by attending pediatric cardiologists if he/she had clinical symptoms compatible with myocarditis and showed at least one of the following: elevated cardiac enzymes (creatine kinase [CK], CK-MB isoenzyme, or troponin-I [>0.1 ng/mL]), cardiomegaly (cardiothoracic ratio >0.5) on chest radiograph, or impaired heart contractility on echocardiography (ejection fraction <55%). Exclusion criterion was underlying congenital heart disease, coronary artery anomalies, cardiomyopathy, collagen vascular disease, infection/inflammation originating from the central nervous system (CNS), or heart surgery. Patients older than 6 years were also excluded for comparison with benign FS. These seven children with myocarditis with seizure-like activity and fever were enrolled to the myocarditis-group. They were initially considered as having FS and reported to our neurologist.
During the same period, children who were diagnosed with benign FS were enrolled to the FS-group. Patients with FS were defined by seizures that occurred between the age of 6 and 60 months with a body temperature of ≥38°C, which were not caused by CNS infection or any metabolic imbalance [9]. Simple FS was presented with a short generalized onset seizure, of duration of <15 minutes, not recurring within 24 hours. Complex FS indicated a focal or generalized onset and/or prolonged seizure, of duration of >15 minutes, recurring more than once in 24 hours, and/or postictal paralysis [9]. Children with status epilepticus, underlying inborn errors of metabolism or chromosomal abnormality, CNS infection and a history of afebrile unprovoked seizures were excluded. Overall, 204 patients were included in the FS-group.
Patients’ demographic profiles, clinical presentations, medical history, vital signs, physical examination findings, and laboratory studies were collected and compared between the myocarditis- and FS-group.
Ethics permission for this study was granted (number: 05-2019-107) by the Institutional Review Board of Pusan National University Yangsan Hospital and fully informed written consent was obtained from each participant.
The SPSS version 19.0 software package (IBM Co., Armonk, NY, USA) was used for statistical analysis of raw scores. The two-tailed chi-square or Fisher’s exact test was used for analysis of categorical data, and the Student’s t-test for continuous variables with normal distribution. The Mann-Whitney U test was used for continuous variables without normal distribution. In addition to univariate non-parametric statistical tests, Fisher’s exact test and the Wilcoxon signed rank test were used to evaluate significant differences in categorical and continuous variables, respectively. In all analyses, P<0.05 was regarded as statistically significant.
Results
1. Clinical features
The myocarditis- and FS-group included seven and 204 children, respectively. Out of 204 FS, the patients of simple FS and complex FS were 152 (74.5%) and 52 (25.5%). There was no significant difference in gender ratio (boy:girl, 2.7:1 vs. 1.6:1) and mean age (2.3±1.2 years vs. 2.6±1.1 years) between simple and complex FS-group (data not shown). There were two boys (28.6%) in the myocarditis-group, and 140 boys (68.6%) in the FS-group (P=0.070) (Table 1). Children in the myocarditis group (4.4±1.9 years) had a substantially older age at onset of seizure-like activities than those of the FS-group (2.4±1.1 years , P=0.033) (Table 1). Body temperature at seizure-like activities onset was significantly lower in the myocarditis-group than in the FS-group (37.9°C±0.2°C vs. 38.7°C±0.6°C, P<0.001). Three patients (42.9%) in the myocarditis-group presented seizure-like activities with fever of <37.8°C, however no children in the FS-group had a seizure with the same degree of fever (Tables 1 and 2). Seizure type was similar between the two groups. Generalized tonic-clonic seizures were the most frequently observed in both myocarditis and FS groups (71.4% and 88.7%, P=0.425). Frequency and duration of seizures were not significantly different between the myocarditis- and FS-groups.

Comparison of clinical and seizure profiles between patients with acute myocarditis and febrile seizure
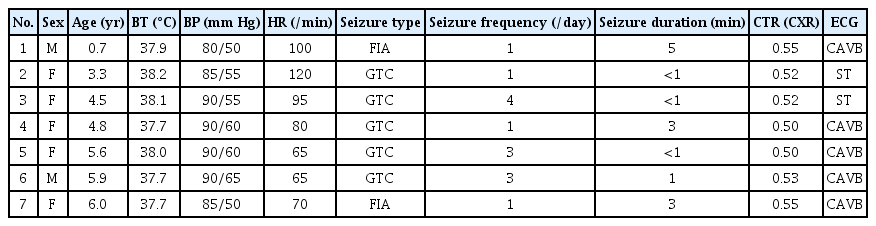
Demographic profiles and clinical presentation of patients with acute myocarditis with seizure-like activities
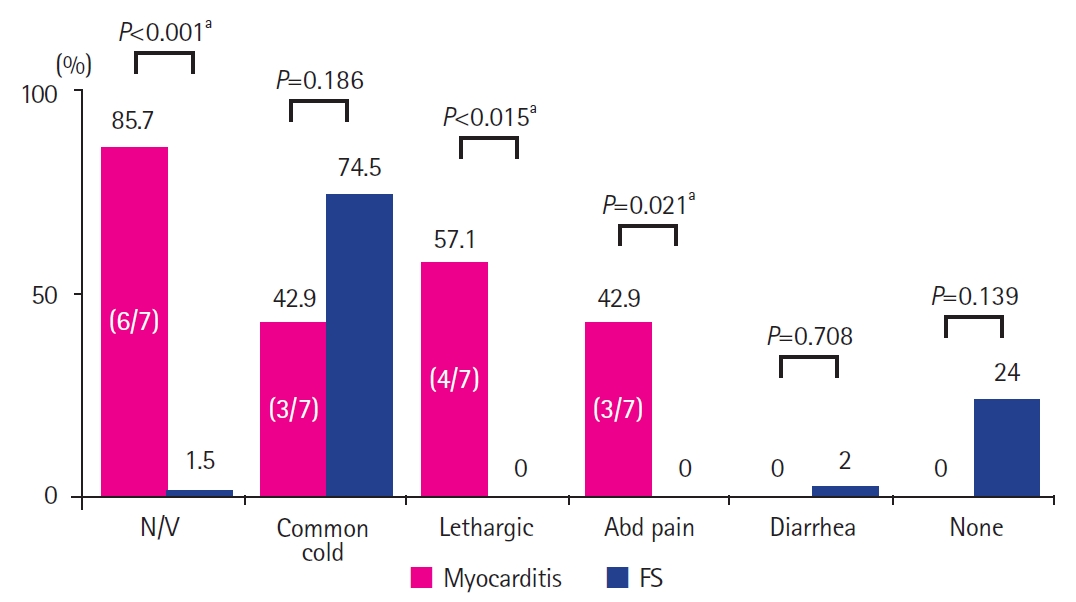
Prodromal symptoms before onset of seizure were statistically different between the two groups (Fig. 1). Nausea/vomiting was the most common symptom in the myocarditis-group (6/7, 85.7%) and was more frequent than in the FS-group (1.5%, P<0.001). Lethargic mentality (57.1% vs. 0.0%, P=0.015) and abdominal pain (42.9% vs. 0.0%, P=0.021) were significantly more common in the myocarditis-group than in the FS-group. Symptoms of common cold, such as cough or rhinorrhea, were more frequently found in the FS-group than in the myocarditis-group (74.5% vs. 42.9%), but this was not statistically significant (P=0.186).
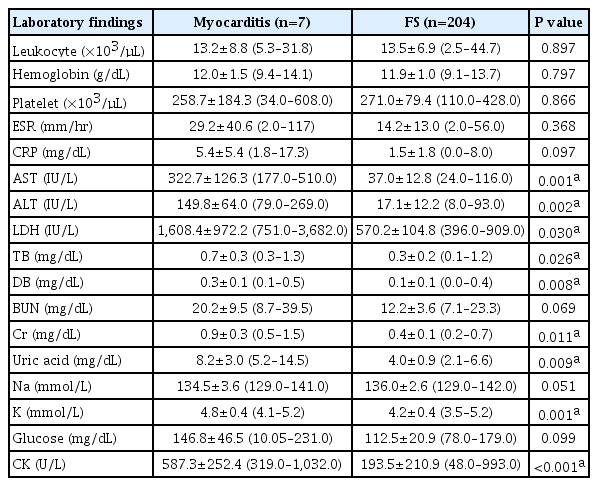
2. Characteristics of initial laboratory results
Initial laboratory findings were significantly different between children in the myocarditis- and FS-groups (Table 3 and Fig. 2). Mean serum levels of chemical profiles were much higher in the myocarditis-group than in the FS-group. Mean levels of aspartate aminotransferase (AST, 322.7±126.3 IU/L vs. 37.1±12.8 IU/L, P=0.0001), alanine aminotransferase (ALT, 149.8±64.0 IU/L vs. 17.1±12.2 IU/L, P=0.002), lactate dehydrogenase (LDH, 1,608.4±972.2 IU/L vs. 570.2±104.8 IU/L, P=0.030), creatinine (0.9±0.3 mg/dL vs. 0.4±0.1 mg/dL, P=0.011), uric acid (8.2±3.0 mg/dL vs. 4.0±0.9 mg/dL, P= 0.009), and CK (587.3±252.4 U/L vs. 193.5±210.9 U/L, P<0.001) were significantly higher in the myocarditis-group than in the FS-group. In particular, the minimum AST level in the myocarditis-group (177 IU/L) was higher than the maximum AST level in the FS-group (116 IU/L) (Fig. 2). Hyperkalemia was more obvious in the myocarditis-group than in the FS-group (4.8±0.4 mmol/L vs. 4.2±0.4 mmol/L, P=0.001). Total blood cell count, ammonia, erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), arterial blood gas analysis, glucose, and electrolyte profiles (except for hyperkalemia) were not significantly different between the two groups.
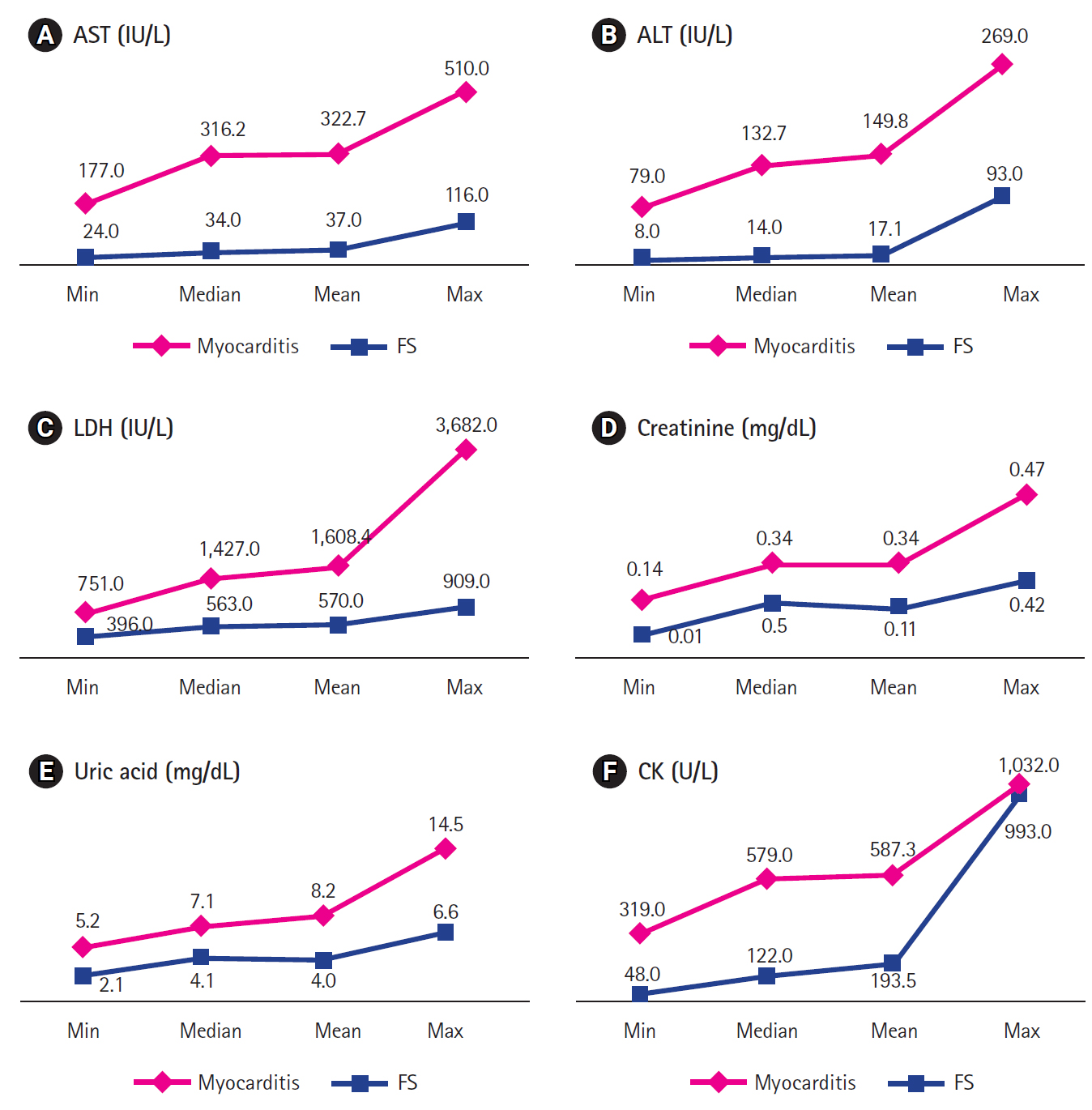
Comparison of laboratory studies between patients with myocarditis and febrile seizure (FS). (A) Aspartate aminotransferase (AST), (B) alanine aminotransferase (ALT), (C) lactate dehydrogenase (LDH), (D) creatine, (E) uric acid, and (F) creatine kinase (CK).
In the myocarditis-group, the mean cardiothoracic ratio on chest X-ray was 0.52±0.24 (Table 2). Two patients (patient 1 and 7) showed definitive cardiomegaly (cardiothoracic ratio ≥0.55), and three patients had a mild increase in cardiothoracic ratio (0.52 to 0.53). Conversely, two patients had no cardiomegaly (patient 4 and 5 ratio, 0.5). Initial 12 lead ECG revealed complete atrioventricular block (CAVB) in five (71.4%) and sinus tachycardia in two patients (28.6%). Of the 204 patients in the FS-group, 172 (84.3%) underwent ECG and showed no abnormal heart rhythm.
Discussion
This study investigated a series of seven children, finally diagnosed with acute myocarditis presenting with seizure-like activity (generalized tonic-clonic seizure or LOC/impaired awareness) and fever, who were initially suspected of having benign FS. Children in the myocarditis-group were significantly older and had a lower degree of fever than those in the FS-group. Although the type, duration, and frequency of seizure were similar between the two groups, the prodromal symptoms/signs were very different. The most common preceding symptom/sign was gastrointestinal problems, including nausea/vomiting and abdominal pain, in the myocarditis-group, and symptoms of common cold in the FS-group. We found that the initial laboratory results in ED were remarkably different between the two groups, even though further cardiac evaluation was not performed. Serum levels of AST, ALT, LDH, bilirubin, creatinine, uric acid, CK, and potassium were higher in the myocarditis-group compared to those in the FS-group. If children have specific prodromal symptoms and considerable elevation in the laboratory findings described, we should consider the possibility of seizure-like activities caused by acute myocarditis, even though these seizure-like activities with fever can look similar to those in benign FS.
As high as 20% to 30% of epileptic seizures may have been misdiagnosed [10]. Some patients may have syncope with convulsion-like involuntary movements, which can be difficult to clinically differentiate from epilepsy. A Stokes-Adams seizure is defined as sudden collapse into unconsciousness due to a heart rhythm disorder, in which there is a slow or absent pulse resulting in diffuse cerebral hypoxia and consequently syncope and/or convulsion [11]. Neglecting a cardiac arrhythmia, which was misdiagnosed as epilepsy, could lead to serious or fatal consequences. In addition, patients may be inappropriately treated with anticonvulsant drugs. Mahoney et al. [12] demonstrated that a Stokes-Adams seizure may be the only clinical manifestation of myocarditis with CAVB. Out of our seven patients with Stokes-Adams seizures, five children showed acute myocarditis with CAVB.
Although many clinicians recognize that resting tachycardia is a common finding of myocarditis due to compensation for congestive heart failure [13], normal heart rates in children with myocarditis were seen in 42% to 66% of patients in two studies [14,15]. For patients with myocarditis with CAVB, bradycardia, rather than tachycardia, is apparent. In our study, none had definitive tachycardia for their age, and in two patients, heart rate was at the low end of the normal range (patient 5 and 6). Since fever and gastrointestinal symptoms usually accelerate a patient’s heart rate, this borderline bradycardia can signal possible cardiac etiology. Carefully and repeatedly checking a child’s heart rate and ECG is very important, especially for those patients with an irregular heart rhythm [15, 16]. Findings on ECG in acute myocarditis are nonspecific and include sinus tachycardia, ST-segment and T-wave abnormalities, abnormal axis, heart block, ventricular hypertrophy, atrial enlargement and decreased voltage [13,15,17]. A 12 lead ECG should be recorded as soon as possible after such a series of episodes and should not be discontinued until an event is captured [18]. Two of our patients in the myocarditis-group had sinus tachycardia in the initial ECG.
Cardiomegaly and/or pulmonary edema are common in patients with myocarditis, but are infrequent in myocarditis complicated with CAVB. Suboptimal heart rate may lead to poor cardiac output before the development of congestive heart failure and cardiomegaly [19]. Wang et al. [20] reported an incidence of 22% for cardiomegaly in children with myocarditis with CAVB. Out of our seven patients, significant cardiomegaly (cardiothoracic ratio ≥0.55) was observed in 28.6%, and two patients showed no cardiomegaly. It should be considered that cardiomegaly may not be present in all myocarditis patients at the onset of the disease.
Modest elevations in liver enzyme levels are found in patients suffering from passive hepatic congestion [21]. A previous report indicated that an ALT/AST ratio >1.0 was seen more frequently with enteroviral perimyocarditis in adult patients [22]. We found that serum levels of AST, ALT, LDH, bilirubin, creatinine, uric acid, CK, and K were significantly increased in the myocarditis-group compared with the FS-group. The levels of AST and ALT were >100 IU/L in all myocarditis patients (except for patient 7, ALT 79 IU/L). In particular, the minimum AST level in the myocarditis-group was higher than the maximum AST level in the FS-group. Elevated levels of AST, ALT and LDH require careful interpretation in patients with myocarditis, because these enzymes are released not only from the liver but also from the skeletal muscles including cardiac muscles. Laboratory cardiac markers including troponin and prohormone of brain natriuretic peptide (pro-BNP) indicate the presence of myocardial damage and dysfunction in myocarditis [15]. Our myocarditis patients showed highly elevated troponin (17.8±9.2 ng/mL, data not shown) and pro-BNP (7,664±8,895 pg/mL, data not shown), which can recognize that our elevation of AST, ALT, and LDH were associated with cardiac damage as well as hepatic congestion. Furthermore, it should be noted that AST and ALT elevations are not specific to myocarditis and occur in other conditions, such as Kawasaki disease, and in conjunction with many viral illnesses. Kawasaki disease is another confusing situation when investigating myocarditis-related seizures. The incidence of FS in the acute phase of Kawasaki disease could be extremely low (0.18%; 95% confidence interval, 0.02% to 0.66%), confirming the results of one meta-analysis report [23]. Although the number of patients is very small, the pattern of FS in Kawasaki disease was usually clustering seizures, focal seizures, and prolonged unconsciousness after seizures [24]. Kawasaki disease has specific diagnostic criteria, including uncontrolled fever of at least 5 days duration, and unique physical findings, with noticeable laboratory findings. None of our myocarditis-group had suspected Kawasaki disease. Other studies demonstrated that patients with acute myocarditis may have an elevated ESR and CRP as inflammatory indicators [4]. In our study, levels of ESR, CRP, arterial blood gas analysis, ammonia, glucose, and electrolyte profiles (except for hyperkalemia) were not significantly different between the two groups. We presume that the change in liver and renal enzyme, CK, and K levels might be more sensitively influenced than those of inflammatory markers such as ESR and CRP, in the early stage of myocarditis. It is encouraging to know that, when typical or atypical FS in children is clinically suspected, initial laboratory findings, especially serum AST, ALT, LDH, bilirubin, uric acid, K, and CK levels, as well as a chest radiograph and ECG, are likely to distinguish myocarditic Stokes-Adams seizure from FS.
Patients with myocarditis may have only nonspecific complaints. Newborns, infants, toddlers, and preschool children may have a history of respiratory or gastrointestinal infection, anorexia, abdominal pain, poor appetite, vomiting or lethargy, seizure-like activity, sinus tachycardia out of proportion to fever, or syncope, whereas cardiac symptoms may be not prominent [8]. These patients are often diagnosed as having gastroenteritis, pneumonia, asthma, or bronchiolitis. Children with gastrointestinal symptoms are commonly given excessive intravenous fluids, which may exacerbate heart failure. At an older age of >10 years old, children may complain of chest pain, exercise intolerance, myalgias, or palpitations, similar to adults reported in the literature [25]. Well-timed diagnosis remains a challenge as children do not always present with typical signs and symptoms of myocarditis.
Of the varied presentations of myocarditis, CAVB was believed to be an isolated feature, with rapid and full recovery if it was diagnosed early and treated with emergency pacemaker implantation [26]. In our study, all except one patient improved their symptoms and signs of low cardiac output within 1 to 4 days after effective pacemaker implantation. One patient (patient 1) died on the 4th day. He had persistent low cardiac output and developed multiple organ failure due to progressive myocarditis, even after inotropic agent and extracorporeal membrane oxygenation therapy. Unless a high level of alertness is maintained, acute myocarditis may easily be missed and diagnosis may only be obvious in cases where fulminant disease is present.
This study has some limitations. First, the study is based on a retrospective investigation of medical records. Second, we acknowledge that there is a large difference in the number of patients between the two groups to make a comparison with the statistical analysis. This is because myocarditis is very rare, and our study enrolled only the children presenting with seizure-like activities and fever among of them. We did try to use the additional non-parametric statistical methods (Fisher’s exact test and Wilcoxon signed rank test) to increase the reliability of statistical analysis. Third, our study aimed to investigate the clinical and laboratory characteristics of the children with myocarditis, whose initial diagnosis could be mistaken for typical or possible FS. Therefore, not all of our myocarditis patients meet typical FS. Finally, these patients were collected at a single tertiary center and the findings may not be completely representative of the general population. Further population-based studies with a larger number of patients are needed.
In summary, children presenting with fever and Stokes-Adams seizure in our study were not diagnosed as having myocarditis at the initial physician encounter, which highlights the need for clinicians to maintain high level of alertness for myocarditis, even in the absence of clinical findings of congestive heart failure. Prodromal symptoms and initial laboratory results revealed significant differences between the myocarditis- and FS-groups. We suggest that an ECG should be considered as a screening test in all episodes of suspicious benign FS in children, especially in those with significant elevations in laboratory findings, including AST, ALT, LDH, uric acid, and CK.
Notes
No potential conflict of interest relevant to this article was reported.
Author contributions
Conceptualization: SON, JAP, SYB, YMK, and YJL. Data curation: SHJ, HDL, JAP, HK, and YJL. Formal analysis: SHJ, JK, and YMK. Methodology: SON, SYB, HDL, and YJL. Project administration: YJL. Visualization: HK and JK. Writing-original draft: SHJ and AK. Writing-review & editing: AK and YJL.
Acknowledgements
This study was supported by a 2018 research grant from Pusan National University Yangsan Hospital. We would like to thank Editage (www.editage.co.kr) for English language editing.