Isolated Unilateral Sixth Nerve Palsy as the First Manifestation of Multiple Sclerosis
Article information
Clinical features of multiple sclerosis (MS) vary widely depending on the area of the lesions. Although brainstem lesions are common in MS, isolated cranial nerve palsies are rare, especially as an initial manifestation [1]. Among the cranial nerves, the fifth nerve is most commonly involved, followed by the 7th, 6th, 3rd, and 8th nerves at MS [1]. Sixth nerve palsy results in ipsilateral horizontal gaze palsy. Common ocular motor symptoms in MS include nystagmus and internuclear ophthalmoplegia (INO) [2]. Unusual ocular motor findings including bilateral 3rd nerve palsy, opsoclonus, and isolated 6th nerve palsy had been reported in MS patients [2]. Here we report the case of a 15-year-old patient who presented with diplopia due to unilateral 6th nerve palsy as the first manifestation of MS.
A 15-year-old man presented with diplopia for 6 days. Physical examination showed limited abduction of the right eye on right lateral gaze. Adduction of the left eye on right lateral gaze was normal (Fig. 1). Other neurological and blood test findings were normal. Magnetic resonance imaging (MRI) of the brain demonstrated multiple ovoid lesions in the periventricular white matter, cerebellum, corpus callosum, basal ganglia, thalamus, pons, and midbrain as a T2 high-signal intensity (Fig. 2). Both gadolinium-enhancing (Fig. 2I) and non-enhancing lesions were present. The lesion in the right pons, which might be in the right sixth cranial nerve pathway, innervated the ipsilateral lateral rectus muscle and might have caused the limited abduction of the ipsilateral eye (Fig. 2B, arrow). MRI of the spine demonstrated T2 hyperintensity and heterogeneous enhancement of the lesions at C4 and C6 (Fig. 2G, H, and J). These findings demonstrated dissemination in time and space. Cerebrospinal fluid (CSF) showed a white blood cell count of 12/mm3 (lymphocyte 99%), 27.9 mg/dL protein, 65 mg/dL glucose, and no bacteria, malignant cells, or oligoclonal bands. CSF immunoglobulin G was elevated (1.95), and antibodies to aquaporin 4 were absent. This patient was not tested antibodies against myelin oligodendrocyte glycoprotein. Ophthalmologic examinations including fundus examination, optical coherence tomography, visual evoked potential, and visual acuity showed normal findings. Brainstem auditory evoked potential and upper and lower extremity somatosensory evoked potentials were normal.

Ocular motility photography. Test of ocular motility demonstrated limited abduction of the right eye at right gaze (A), esotropia of the right eye at primary position (B), and normal ocular motility at left gaze (C). The consent was obtained from the patient and the guardians regarding the publication of the patient’s images.
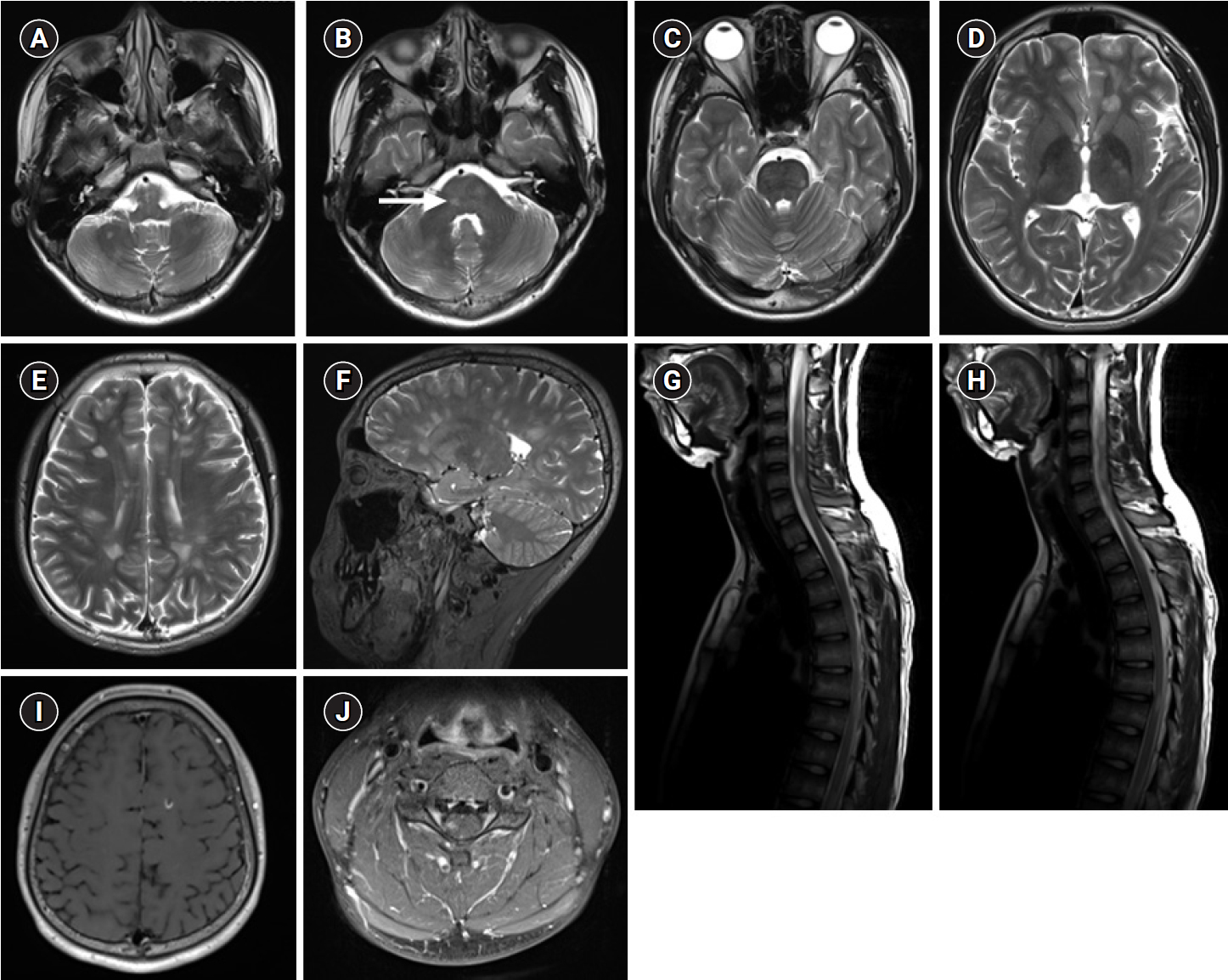
Magnetic resonance imaging (MRI) of the brain demonstrates multiple ovoid lesions in the cerebellum (A), pons (B, arrow), midbrain (C), basal ganglia, thalamus (D), and periventricular white matter (E, F), as a T2 high-signal intensity. MRI of the spine demonstrates T2 hyperintense and heterogeneous enhancing lesions at C3, C4, C6 (G) and T7 (H). MRI of gadolinium-enhanced T1-weighted images demonstrates several lesions in the frontal lobe (I) and C4 (J).
Based on the 2017 McDonald criteria, the patient was diagnosed with MS; one attack and two or more lesions on MRI demonstrating dissemination in time and space. He was treated with intravenous (IV) methylprednisolone (1 g/day) for 5 days, which he did not respond to, followed by oral prednisone (1 mg/kg/day, tapered over 5 weeks). Therefore, IV immunoglobulin (2 g/kg divided over 4 days) was administered, but the lateral rectus muscle dysfunction did not improve. Subsequently, he received a plasma exchange five times in 10 days and had marked improvement in diplopia and the lateral rectus muscle function; Grading of abduction was improved from –4 (no movement beyond the midline) to –1 (75% of movement remains). He has been receiving interferon-β 1b subcutaneously since the 5 days after the last plasma exchange. Interferon-β 1b was titrated to 0.25 mg (8 million IU) every other day. At the 7-month follow-up, the 6th cranial nerve palsy had completely resolved. No neurological symptoms had occurred until the 14-month follow-up. Follow-up MRIs of the brain and spine revealed a slight decrease in the lesion size.
INO is a common ocular motor symptom in MS, affecting 30% of cases [3]. INO is an eye movement disorder caused by a lesion of the medial longitudinal fasciculus (MLF), which affects conjugate eye movement by connecting the paramedian pontine reticular formation (PPRF)—abducens nucleus complex of the contralateral side to the oculomotor nucleus of the ipsilateral side [3]. The MLF lesion impairs the adduction of the affected eye during contralateral gaze, while the contralateral eye abducts but is accompanied by nystagmus. If the lesion is located in the PPRF, abducens nucleus, or contralateral MLF, conjugate horizontal gaze palsy to the ipsilateral side occurs instead of ipsilateral lateral gaze palsy.
Our patient presented with limited abduction of the unilateral eye and intact conjugate adduction of the contralateral eye. This indicated that the pathologic lesion involved the 6th nerve alone, and not the abducens nucleus, PPRF, or MLF [4]. Isolated 6th nerve palsies are rare, seen only in 0.4% to 1.0% of MS [1]. There have been no reports of isolated sixth nerve palsies in children, so they might be even rarer.
After MS diagnosis, aggressive acute management including steroid, immunoglobulin, and plasma exchange was provided in a timely manner, leading to complete resolution of the 6th nerve palsy. Interferon-β was initiated in the early period and has been maintained without complications and relapses.
Incomplete recovery indicates poor prognosis, and early, effective treatment of MS prevents irreversible long-term complications [5]. Although isolated 6th nerve palsies are rarely observed in MS, especially in children, MS should be a differential diagnosis.
Notes
No potential conflicts of interest relevant to this article was reported.
