|
 |
- Search
| Ann Child Neurol > Volume 27(2); 2019 > Article |
|
Rotavirus is an important cause of severe gastroenteritis in infants and children. Generally, rotavirus infections are self-limiting benign diseases but occasionally can cause a wide range of neurological manifestations, including benign febrile or afebrile convulsions, meningoencephalitis, cerebellitis, and lethal encephalitis or encephalopathy [1]. However, it is unclear how rotavirus can affect the central nervous system without direct invasion.
Posterior reversible encephalopathy syndrome (PRES) is a well-recognized clinical disorder with typical neuroimaging findings consisting of mostly transient bilateral gray and white matter abnormalities in the posterior cerebral hemispheric regions and cerebellum [2]. The common clinical symptoms are headache, confusion, seizures, and visual disturbances such as cortical blindness. These symptoms usually recover without sequelae following appropriate treatment. Common precipitants are sudden elevations of blood pressure, renal failure, fluid restriction, and treatment with immunosuppressive drugs such as cyclosporine [3]. Recently, studies related to infection-associated PRES have been published [2,4]. We describe the case of a 6-year-old boy with rotavirus gastroenteritis who developed clinical and radiological manifestations consistent with PRES.
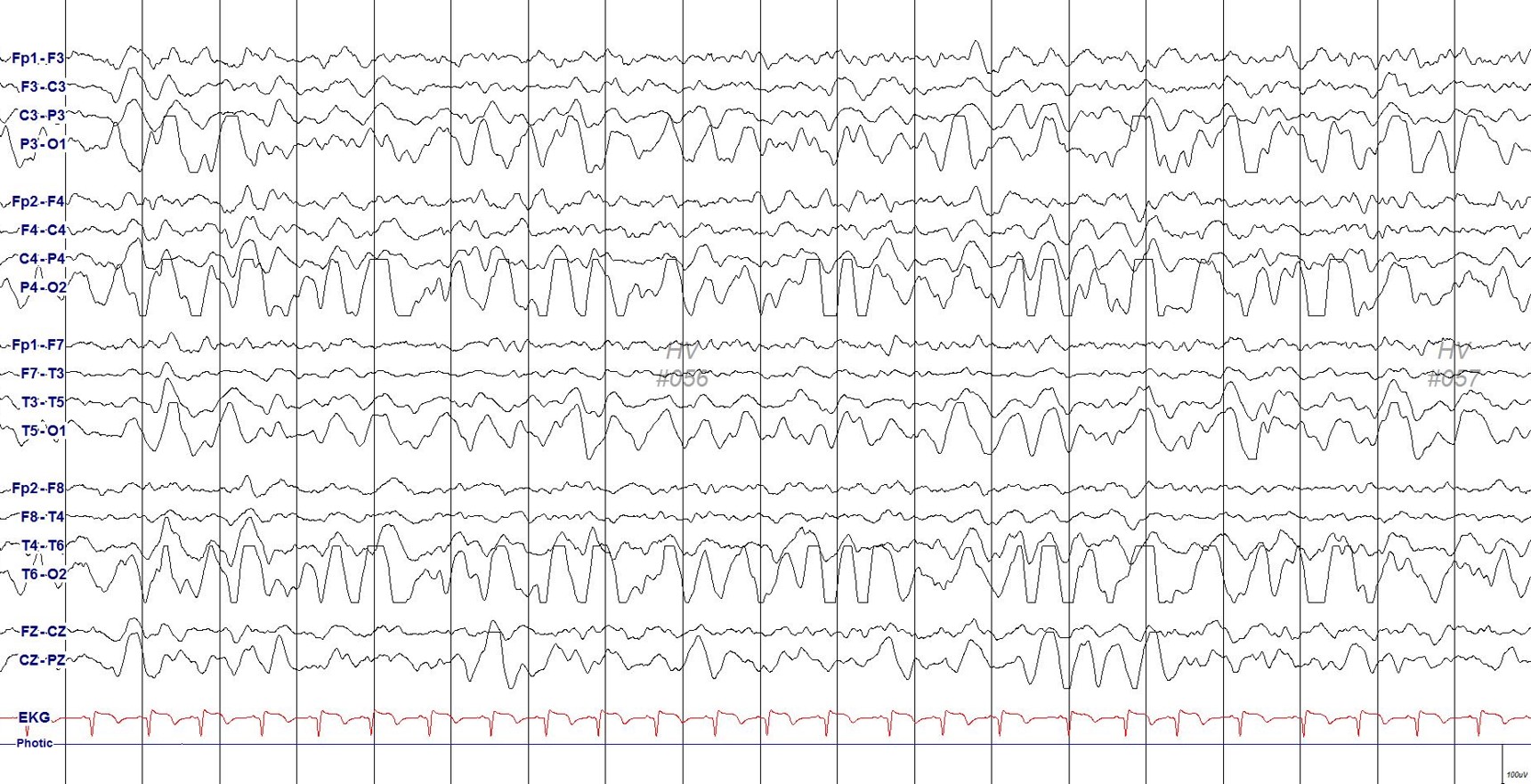
A previously healthy 6-year-old boy was referred to the pediatric emergency room with a 4-day history of vomiting and abdominal pain despite being treated with fluid therapy at a private clinic. His development was normal, and his past medical history was unremarkable. On examination, the patient was conscious, mildly dehydrated, and afebrile. At the time of admission, his blood pressure was 110/70 mm Hg (normal range, 97 to 115/57 to 76) and heart rate was 90 beats/minute (normal range, 75 to 118). The boy experienced sudden visual and consciousness disturbances on the day of hospital admission for fluid treatment. A few hours later, he had a generalized tonic convulsion for 3 minutes without definite fever. The results of a routine blood test at that time showed no abnormalities except for mildly elevated inflammatory markers: white blood cell count, 16.3├Ś103/╬╝L; hemoglobin, 14.9 g/dL; platelet count, 426├Ś103/╬╝L; total CO2, 26.7 mmol/L; sodium, 134 mEq/L; potassium, 3.7 mEq/L; chloride, 98 mEq/L; C-reactive protein, 1.40 mg/dL; glucose, 151 mg/dL; ammonia, 26 ╬╝mol/L; and calcium ionized, 1.23 mmol/L. His blood pressure increased slightly to 133/85 mm Hg but remained relatively stable. A cerebrospinal fluid analysis revealed no pleocytosis and was negative for viruses. Immediate brain magnetic resonance imaging (MRI) demonstrated bilateral multifocal patchy (more prominent in the left) increased fluid attenuated inversion recovery (FLAIR) signal intensity (negative on diffusion-weighted MRI) at both occipitoparietal cortices, and some nearby white matter areas exhibited slight obliteration (Fig. 1). Rotavirus antigen was detected in a stool specimen by latex agglutination. Parents remembered that their child had not been vaccinated with rotavirus and this was the spring of the epidemic of rotavirus infection. Electroencephalography showed semirhythmic high amplitude 1.5 to 2 Hz delta activities on both occipital areas (Fig. 2).
We immediately administered intravenous methylprednisolone (30 mg/kg/day for 3 days) and continued conservative treatments. MRI taken 12 hours later showed interval resolution of previously noted vasogenic edema, gyral swelling, and decreased FLAIR signal intensity (Fig. 1). His clinical condition improved over the next 2 days. Visual evoked potential testing revealed a delay of evoked potential latencies in the left eye. He was discharged on hospital day 10 without any neurologic complications. Two weeks later, follow-up brain MRI showed that the previous lesions were disappeared (Fig. 1).
In this case, rotavirus gastroenteritis developed in a patient who was older than most patients with rotavirus. Convulsive symptoms related to rotavirus infection may occur as PRES without definite fluctuation of blood pressures. Approximately one-third of patients with PRES have normal or only mildly increased blood pressure, though most are hypertensive [4,5]. PRES is an increasingly recognized disorder readily diagnosed via brain MRI in clinical practice. There is a wide clinical spectrum of both symptoms and triggers, and yet it remains incompletely understood. The most widely accepted theory is that severe hypertension interrupts brain autoregulation [5]. In patients with impaired cerebral autoregulation, uncontrolled hypertension leads to hyperperfusion and cerebral vessel damage, which can cause fluid to leak into the brain parenchyma, eliciting vasogenic edema [5]. However, as mentioned earlier, a significant proportion of patients do not demonstrate hypertension. An alternative theory is that systemic inflammation causes endothelial dysfunction [4]. In a systemic inflammatory process such as sepsis, eclampsia, transplantation, and autoimmune disease, the vasoconstriction that occurs during autoregulation could exacerbate pre-existing inflammatory endothelial dysfunction, causing hypoxia and subsequent vasogenic edema [5]. We can explain why a typical PRES without hypertension developed in this case of infection-associated PRES. However, we are not sure whether age affected the patientŌĆÖs symptoms. There have been only two cases reported so far: parainfluenza virus infection in an adult and rotavirus infection in an infant [4,5]. In other words, infection-associated PRES, as well as hypertension-associated PRES, contribute endothelial dysfunction to the pathophysiology of this clinical-radiological syndrome.
In summary, this case describes a patient with rotavirus infection-associated PRES with a good prognosis. Pediatricians should be well aware that rotavirus gastroenteritis-induced convulsions have a wide spectrum and may be related to reversible posterior leukoencephalopathy. Prompt diagnosis and treatment, including stopping precipitating factors when possible, are crucial to achieving good reversibility.
Fig.┬Ā1.
Brain magnetic resonance imaging (A, B) axial fluid attenuated inversion recovery (FLAIR) obtained 12 hours after the onset of symptoms showing bilateral multifocal patchy hyperintensity at the both parietooccipital, left high frontal cortex, and some nearby white matter areas. Axial FLAIR (C) obtained 24 hours after the onset of symptoms showing interval resolving previous vasogenic edema, gyral swelling, and hyperintensed lesions, and axial T2-weighted imaging (D) revealed normal finding. After 2 weeks, axial FLAIR (E) and T2-weighted imaging (F) showed interval normalized, disappeared previous lesions.

References
2. Celik T, Celik U. Posterior reversible leukoencephalopathy syndrome with rotavirus gastroenteritis. J Pediatr Infect 2015;9:126-9.

3. Endo A, Fuchigami T, Hasegawa M, Hashimoto K, Fujita Y, Inamo Y, et al. Posterior reversible encephalopathy syndrome in childhood: report of four cases and review of the literature. Pediatr Emerg Care 2012;28:153-7.


- TOOLS
-
METRICS

- Related articles in Ann Child Neurol
-
Clinical Spectrum of Posterior Reversible Encephalopathy Syndrome in Children2020 April;28(2)
Two Cases of Influenza-associated Encephalopathy.2005 May;13(1)